Brooklyn Physical Therapy News- Evolve NY
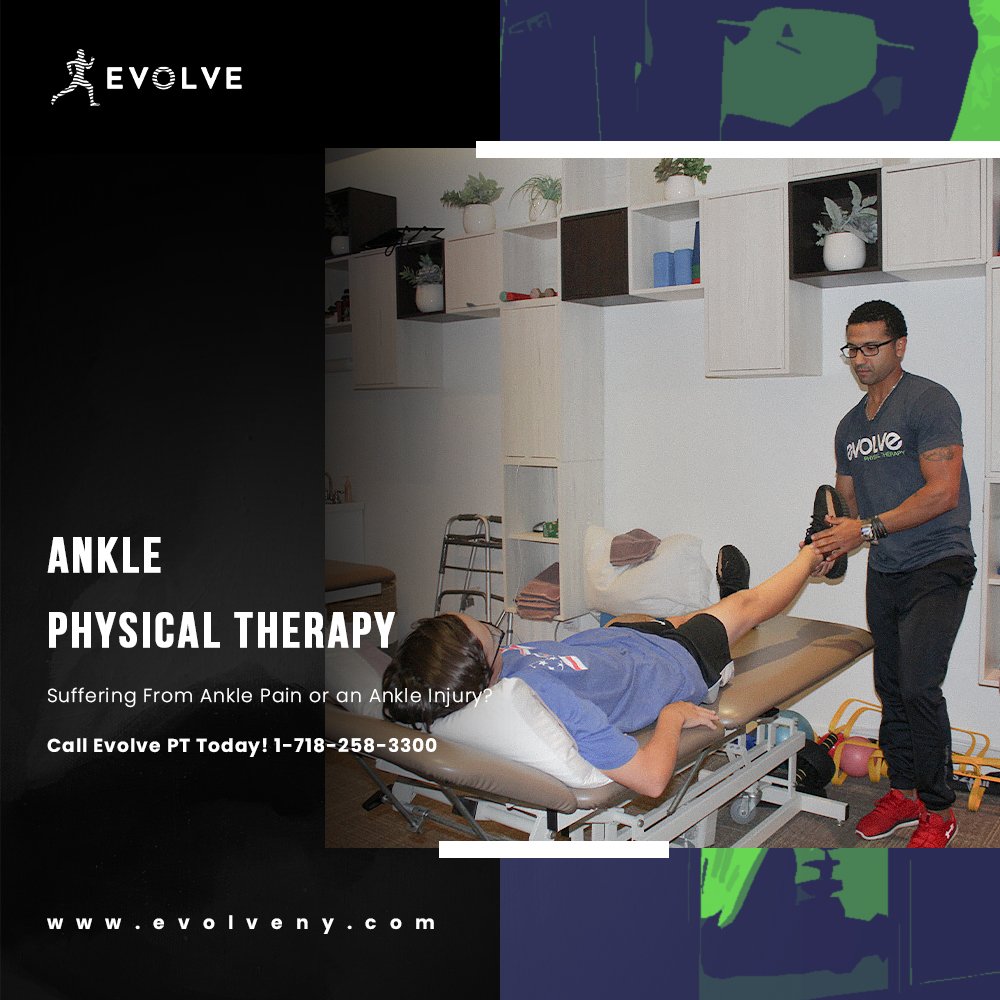
Addressing Ankle Pain with Physical Therapy
Addressing Ankle Pain with Physical Therapy: What a Pain in the Ankle! Looking for Answers to Ankle Pain? Ankle pain, whether new or chronic, can seriously interfere with being on your feet. If sitting down all day isn’t an option, physical therapy is a great choice for identifying the cause of your ankle pain and taking steps to getting a handle on your symptoms…
What a Pain in the Ankle!
Looking for Answers to Ankle Pain?
Ankle pain, whether new or chronic, can seriously interfere with being on your feet. If sitting down all day isn’t an option, physical therapy is a great choice for identifying the cause of your ankle pain and taking steps to getting a handle on your symptoms.
LET’S EXAMINE THE ANKLE CLOSER
The ankle is a hinge joint where the primary motion is to lift and point the foot. If we look at an image of the ankle joint you will see the larger inner bone of the lower leg leg called the tibia and the thinner outer bone called the fibula articulate with a bone called the talus in the posterior part of the foot. Beneath the talus lies the calcaneus or heel bone. Many ligaments, muscles. and tendons travel between the bones of the lower leg and foot, crossing the ankle joint.
Because of the complex anatomy in the ankle area, there are many potential sources of ankle pain or discomfort. In this article we will take a look at some of the more common causes of pain and how physical therapy can treat these conditions.
COMMON CAUSES OF ANKLE PAIN
Posterior Ankle Pain
Posterior Ankle Impingement: symptoms of this condition include posterior ankle pain with forced plantarflexion (pointing of the toe or pushing off of the toe). It results from compression of the soft or bony tissue between the tibia and the calcaneus. Some people have a small extra bone in their ankle called an O’s Trigonum which can increase the compression. On occasion a large amount of force through the ankle joint can cause small fragments of bone to fracture and become compressed when the toe is pointed. Inflammation and swelling in this area leads to pain.
Achilles tendinopathy or rupture: pain felt behind the heel and up the back of the ankle may indicate an irritation of the achilles tendon, the long tendon that connects the calf muscles to the bottom of the foot. This irritation may be a result of an acute or sudden trauma or from repetitive microtrauma and can cause discomfort when walking, running, jumping, or climbing stairs. Tenderness when pressing the achilles tendon, stiffness and pain especially during first steps, and swelling in the back of the ankle are characteristic of this condition. In the case of a tendon rupture or tearing of the tendon, calf weakness, bruising, swelling, and pain result. A full rupture can typically be identified by squeezing the calf muscle with your hand and observing a lack of toe pointing indicating the connection between the calf muscle and foot has been disrupted.
Lateral Ankle Pain
Ankle sprain: rolling your ankle outward, can cause an acute ankle inversion sprain. There are three ligaments on the outside of the ankle that can be injured when stretched beyond their normal capacity. These ligaments are the anterior talofibular ligament (ATFL), the calcaneofibular ligament (CFL) and the posterior talofibular ligament (PTFL). Tenderness over the involved ligament is common. Depending on the severity of the sprain you may notice bruising, swelling, stiffness, and if the sprain is severe, laxity or instability of the ankle.
Peroneal tendon injury: Two peroneal muscles run along the outer lower leg and their tendons travel behind the ankle bone (known as the lateral malleolus) and attach at the outer midfoot and beneath the foot. These muscles are tasked with stabilizing the foot and helping to prevent sprains and injuries. Symptoms of peroneal tendon injury can come on suddenly or over time and include pain or tenderness along the lateral lower leg or ankle. Warmth or swelling may be noticed in the lateral ankle and a pop may be heard with a sudden injury. Increases in activities such as running, jumping or walking, a sudden trauma to the ankle, having high arches and wearing inappropriate footwear can contribute to this type of injury
Sinus Tarsi Syndrome: this clinical syndrome is characterized by pain in the lateral foot just below the ankle in an area called the sinus tarsi. It is thought to be caused by inflammation and scar tissue formation possibly brought on by abnormal mechanics in the joint between the talus and calcaneus. Recurrent ankle sprains causing instability may be a predisposing factor.
Medial Ankle Pain
Ankle sprain: rolling the ankle inward so that the outer edge of the foot lifts up is called an eversion sprain. The primary ligament involved in this type of sprain is called the deltoid ligament, a strong, flat, triangular band composed of four separate ligaments. Tenderness over the deltoid ligament is common with this type of injury. Depending on the severity of the sprain you may notice bruising, swelling, stiffness, and if the sprain is severe, laxity or instability of the ankle.
Medial ankle stress fracture: a stress fracture refers to a weakening of one area of bone caused by repetitive breakdown of bone without sufficient rebuilding. It is considered an overuse injury and seen most commonly in track and field athletes and military recruits who walk long distances with heavy packs. In the ankle, pain and tenderness along the inner ankle bone called the medial malleolus may indicate a tibial stress fracture. Initially the pain is present during activity and will improve with rest but over time it may become more constant and be accompanied by tenderness to touch over the area and swelling or bruising.
Posterior tibial tendonitis: The tibialis posterior muscle runs along the inside of the calf muscle and its tendon travels behind the medial ankle bone and attaches under the arch of the foot. Pain or swelling along the inner ankle or arch of the foot especially with standing or walking and increased pronation or flattening of the arch are common with this condition. Overuse or sudden trauma can trigger this condition
Tarsal Tunnel Syndrome: Running parallel to the tendon of the posterior tibialis, the tarsal tunnel is a dense band of fibrous tissue that creates a tunnel through which the tibial nerve, several tendons, and the blood vessels traveling to the foot, course. Similar to carpal tunnel in the wrist, compression of the tibial nerve as it passes through the tarsal tunnel can cause burning, tingling, electrical shock pain, and numbness in the inner ankle and/or bottom of the foot
Anterior Ankle Pain
High ankle sprain: In contrast to the much more common lateral ankle sprain, the high ankle sprain involves injury to the ligaments that connect the tibia bone to the fibula bone just above the ankle. This ligamentous connection helps stabilize the ankle joint and typically has very minimal movement so a large force is needed to disrupt and injure this area. It is important to correctly diagnose this injury as it typically requires longer times to heal and can result in more chronic ankle instability than other ankle sprains.
Anterior Ankle Impingement: Ankle instability, bone spurs, and repeated stress at end range positions of squatting, jumping, or descending stairs can cause this condition that leads to pain in the anterior aspect of the ankle. A history of repeated ankle sprains may predispose one to this condition as scarred ligaments take up more room in the joint space leading to compression and inflammation.
PHYSICAL THERAPY FOR ANKLE PAIN
Identifying the cause of your pain is the first order of business when a physical therapist assesses your ankle. If your physical therapist suspects a more serious injury such as a tibial stress fracture or high grade ankle sprain they may refer you back to your doctor for imaging to determine if surgery, modifications to weight bearing, bracing, or casting are needed.
If you are being treated for an acute injury such as a tendon injury or sprain, your physical therapist will educate you on how to protect these newly healing tissues. Treatment may include compression or bracing, offloading the injured area through crutches, modalities such as ice, ultrasound or electrical stimulation to reduce pain and swelling, and activity modification.
In the case of well-healed tissues, chronic injuries like tendinopathy or ankle impingement, or a well-healed stress fracture your physical therapy program will focus not only on reducing or eliminating localized symptoms but on addressing factors that contributed to the onset of the symptoms. Often chronic injuries or pain in the ankle are caused by repeating faulty movement patterns or having an imbalance of muscle strength and length to carry out a task such as walking, running,or jumping. Optimizing muscle strength and flexibility and improving motor control and mechanics of the lower limb is important for returning to prior activities and reducing the likelihood of the injury recurring.
While some ankle injuries may require intervention by a doctor or surgeon, a physical therapist should always be a primary member of your care team. A physical therapist at Evolve can help you get on the road to recovery. Our therapists do not just treat symptoms, but we get to the root of the cause. We strive to enable our patients to live pain free, and prevent the recurrence of related issues
Click here for more information about physical therapy for your ankles!
About EvolveNY-
Brooklyn's Premier Holistic Physical Therapy Clinics- There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
Look out Gravesend, Evolve Physical Therapy is Coming Your Way
Evolve Physical Therapy is Growing to Gravesend! And Gravesend Makes Four: Evolve Physical Therapy Opens a New Location in Brooklyn. Check it out, Brooklyn, Evolve Physical Therapy + Sports Rehabilitation is growing! We are very excited to announce a brand new flagship location in Gravesend on Avenue U. Construction is wrapping up as we speak and we are thrilled that we will have the opportunity to serve more of our community members…
Evolve Physical Therapy is Growing to Gravesend!
And Gravesend Makes Four: Evolve Physical Therapy Opens a New Location in Brooklyn
Check it out, Brooklyn, Evolve Physical Therapy + Sports Rehabilitation is growing! We are very excited to announce a brand new flagship location in Gravesend on Avenue U. Construction is wrapping up as we speak and we are thrilled that we will have the opportunity to serve more of our community members.
Since our first location opened its doors in 2010, Evolve Physical Therapy + Sports Rehabilitation has been providing physical therapy, post-operative care and pain relief to the people of Brooklyn. After hearing so many experiences of unsuccessful physical therapy treatment we knew it was time to get to work. We have always believed that long term health and recovery is achievable through physical therapy and we set forth to build a model of care that is holistic, patient-centered and focuses on addressing the root cause of pain and injury, and the dysfunction they are causing.
If you’ve been to our Marine Park, Mill Basin, or Park Slope locations already then you know how much detail and attention we put into designing our clinic spaces. Our new Gravesend location is no exception and we can assure you this place will look good. But more importantly you will feel great after working with one of our skilled therapists who will provide you with the one on one attention that quality physical therapy care necessitates.
From pediatrics to post-surgical care, neurologic rehab to sports injury recovery, we’ve got a team member ready to get you on the road to recovery. Let us show you what high quality physical therapy care looks like when provided by a team of therapists passionate about their profession and the impact they can make on the people of New York.
Follow us on social media @Evolvefit4life to get a sneak peak at our progress and be the first to know when it’s time for the official grand reveal! Click here to find out more information about our new HQ location- https://evolveny.com/locations/gravesend-physical-therapy-brooklyn
About EvolveNY-
Brooklyn's Premier Holistic Physical Therapy Clinics- There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
https://EvolveNY.com
Rotoscoliosis: A Twisted Tale of the Spine
Rotoscoliosis: A Twisted Tale of the Spine- Are You Living With Rotoscoliosis? The human skeleton is designed to be balanced and aligned so that our muscles, tendons, ligaments, and organs can work optimally. But variation still exists within the bones and joints of individual skeletons. In some cases these variations go unnoticed unless picked up incidentally on imaging.
Are You Living With Rotoscoliosis?
The human skeleton is designed to be balanced and aligned so that our muscles, tendons, ligaments, and organs can work optimally. But variation still exists within the bones and joints of individual skeletons. In some cases these variations go unnoticed unless picked up incidentally on imaging. In other cases they are visible to the naked eye and can affect the functioning of the body in small and large ways. In this article we will be discussing a condition of the spine that can have large implications on movement and daily functioning called rotoscoliosis.
LET’S TAKE A LOOK AT THE SPINE ITSELF
Balance between stability and mobility allows the spine to keep you standing tall but allows you the flexibility to bend, twist, and arch your back. Whether you are reaching down to pick your child up from the floor or hitting a hole-in-one on the golf course, appropriate spinal alignment and flexibility are essential. Let’s take a closer look at the anatomy of the spine.
The spine is made up of five distinct segments. The seven vertebrae that make up the neck, known as the cervical spine, the 12 vertebrae that make up the mid back, or thoracic spine, and the 5 vertebrae that make up the lower back, or lumbar spine, create a long canal that houses the spinal cord. The broad and flat sacral bones sit beneath the last lumbar vertebrae and act as connectors between the pelvic bones and the spine. Beneath that, lies the coccyx or tailbone.
If you look at a model of a typical, healthy spine from the back or front it appears to be a straight column of vertebrae stacked on top of one another. When you view the spine from the side, however, you will see that the spine is actually curved in several places. In the neck the spine curves toward the front creating a small arch or “lordosis” in the neck. It then switches directions and a gentle backwards curve or “kyphosis” can be seen in the thoracic spine followed by another reversal and lordosis in the lumbar spine. Even the sacrum and coccyx are slightly curved. This normal alignment of the spine allows for all of the movement we expect from the spine, proper shock absorption capabilities, and good alignment from the head to the feet.
WHAT IS ROTOSCOLIOSIS?
Scoliosis is an abnormal curvature of the spine. It affects about 2% of women and 0.5% of men and can begin in infancy, childhood, adolescence, or adulthood. While a certain amount of curvature in the spine from front to back is normal, curvature that goes from left to right is characteristic of scoliosis. Several subsets of scoliosis exist based on the location of the abnormal curvature and its characteristics. Rotoscoliosis is used to define one of the most severe forms of scoliosis. The name comes from the word “rotation”. In this type of scoliosis the vertebral column is both curved toward the side and rotated. All scoliosis has a degree of rotation or twisting of the spine but in rotoscoliosis it is severe.
Scoliosis can be congenital, meaning it is present before birth (usually caused by abnormal formation of spinal bones)--or idiopathic, in which case it develops after birth. The cause of a scoliosis can typically be identified as one or more of three causes. A functional scoliosis develops in response to a skeletal or movement abnormality elsewhere in the body. For example, a discrepancy in length between the legs could cause a functional scoliosis to develop because the hips are not even. A scoliosis can also be neuromuscular in origin meaning it is associated with a condition that affects the nerves or the muscles. Finally degeneration of the vertebral bodies and weakening of their supporting ligaments can cause scoliosis to develop in adults.
HOW IS THIS CONDITION IDENTIFIED?
If scoliosis is mild it may be hard to identify without an X-ray, CT, or MRI of the spine. If moderate or severe, the following are visible signs that may indicate scoliosis:
-One shoulder is higher than the other
-One hip is higher than the other
-A “rib hump” can be seen on one side of the back as the person bends forward
-One shoulder blade is more prominent than the other
-The spine appears twisted
-Clothing appears to hang unevenly
Radiologists use certain measurement techniques to quantify the degree of curvature of a rotoscoliosis. This allows them to monitor progression over time and to guide treatment decisions.
HOW DOES IT FEEL?
A mild rotoscoliosis may not cause any symptoms. As the rotation and sidebending of the spine increase, discomfort or pain in the back or rib cage may develop. A person may notice changes in their walking gait or in their ability to perform daily tasks like reaching, bending, or even sleeping. If the degrees of curvature and rotation are severe enough, the heart and lungs can even be affected. With the changes in rib cage position, taking a full breath may become restricted.
WHAT CAN BE DONE?
Observation: In young children with a mild scoliosis observation may be the first course of treatment. If a child has a mobility impairment it can be helpful to use proper positioning equipment to make sure their spine is aligned optimally, for example while they are sitting to help limit curvature and rotational progression.
Physical Therapy and Exercise: Advances in conservative treatment for scoliosis have come a long way. Exercise and physical therapy are important tools to help manage a condition like rotoscoliosis. At Evolve, we utilize the Schroth Method, a physical therapy technique that can help stop the progression of scoliosis and has been proven to reduce pain.
Bracing: Bracing is often helpful in stopping the progression of skeletal maturity in those with moderate scoliosis who have not yet reached skeletal maturity. Bracing is customized to fit the individual’s body and needs to be regularly reassessed to ensure proper fit. They may need to be worn for 16-23 hours a day until skeletal maturity is reached.
Surgery: Surgical intervention to straighten and stabilize the spine may be recommended in children with severe curvature and adults with severe curvature who are also experiencing signs of nerve damage or compression such as leg weakness and bowel or bladder issues.
The appropriate treatment measures for your rotoscoliosis should be decided upon by you and your physicians. Whether observation, bracing, or surgery is the route you are taking, physical therapy can be an important treatment strategy to improve your pain, slow the progression of rotoscoliosis, and help maximize your ability to participate in all the activities of daily life.
Click here to find out more information about scoliosis treatments in Brooklyn
About EvolveNY-
Brooklyn's Premier Holistic Physical Therapy Clinics- There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
https://EvolveNY.com
Gout Got You Down?
Are you suffering from gout? Physical Therapy Can Help–many people have heard of it but for the more than 8 million people in the U.S. suffering from gout, it is a painful reality they’d love to prevent. While medical care from a physician is an important part of managing gout, many people do not know that a physical therapist can help address the symptoms and risk factors associated with gout…
Physical Therapy for Gout
Are you suffering from gout? Physical Therapy Can Help
Gout–many people have heard of it but for the more than 8 million people in the U.S. suffering from gout, it is a painful reality they’d love to prevent. While medical care from a physician is an important part of managing gout, many people do not know that a physical therapist can help address the symptoms and risk factors associated with gout.
WHAT IS GOUT?
So what is gout? Gout is a complex form of arthritis characterized by sudden, severe bouts of joint swelling, pain, warmth, redness, and tenderness. Accumulation of needle-like urate crystals in the joint causes the inflammation and pain characteristic of gout.
Urate crystals form when either too much uric acid is produced by the body or too little is excreted by the kidneys. Uric acid is produced normally by the body when it breaks down what are called purines. Purines are substrates found commonly in food we eat such as red meat, organ meat and some seafood like tuna, anchovies, and mussels. Eating these foods in high amounts can cause elevated uric acid as can drinking certain alcohols such as beer or sugary cocktails.
Men tend to be at higher risk for developing gout than women, though post-menopausal women are at a higher risk than their pre-menopausal counterparts. Certain medications such as low dose aspirin, ACE inhibitors and anti-rejection medications for post-organ transplant patients may increase levels of uric acid in the body. Finally, a family history of gout and a personal history of certain medical conditions such as obesity, uncontrolled high blood pressure, diabetes, metabolic syndrome, or heart and kidney disease increase one’s risk of developing gout.
Gout attacks are most common in the joint at the base of the big toe but can actually occur in any joint. Ankles, knees, fingers, wrists and elbows may be affected by gout as well. An attack of gout typically occurs suddenly. You may awake in the middle of the night with pain, heat, and redness in a joint so severe that even the bedsheet touching the area is unbearable.
It is important to call your doctor if you develop these symptoms. Firstly it is important to rule out other causes of joint pain, redness and swelling such as an infection or acute injury. Secondly, untreated gout can lead to joint erosion and prolonged pain.
HOW IS GOUT TREATED?
During an acute gout attack your physician may prescribe medications to reduce inflammation and manage pain. They may also recommend medications to prevent the build-up of uric acid and improve its removal from the body to decrease your risk of future gout attacks.
While your physician is an important and necessary first point of contact for treating gout, a physical therapist should be another important member of your care team.
WHAT IS A PHYSICAL THERAPIST’S ROLE IN TREATING GOUT?
Once the gout attack is under control, physical therapy is a great option to help restore normal joint movement and function and also to address lifestyle modifications that will lower your risk for future gout attacks.
Lifestyle modifications: If you go back and review the list of risk factors for gout outlined above, you will notice that many of them can be addressed with modifications to one’s lifestyle. It should feel empowering to know that medication is not the only way you can decrease the likelihood of another gout attack and of developing long term joint damage.
Participation in a regular exercise program consisting of moderate to high intensity cardiovascular and strength training can improve risk factors for diabetes, heart disease, high blood pressure, and metabolic syndrome, all conditions associated with an elevated risk for gout.
For many people, lack of familiarity with exercise and concerns about injury or worsening pre-existing conditions such as joint pain or heart disease is a barrier to entry for exercise. Luckily, physical therapists are experts in prescribing exercises that are individualized to not only prevent worsening of your pre-existing medical concerns but to actually help improve them! When you work with a physical therapist they can advise you on how to safely begin an exercise program. Your physical therapist will take the time to get to know your medical history, your current abilities, your concerns, and your motivating factors and help tailor a program to meet your needs.
Physical therapy treatment: Physical therapy for gout will focus on managing pain symptoms and improving function. Modalities such as cryotherapy (cold/ice) have been shown to improve inflammation and pain during a gout attack. Your physical therapist may advise you on splinting, or bracing the involved joint or on assistive devices such as a cane or crutches when pain is severe enough to impair walking.
As the acute attack wanes or in the case of chronic joint damage from gout, restoring normal joint motion is an important part of restoring your function. Your PT may apply gentle hands-on techniques such as passive range of motion, soft tissue therapy or joint mobilization, myofascial release techniques, or taping to improve the mobility and health of the joint and soft tissues that are affected.
In the case of chronic gout, while the surfaces of the joint may no longer be pristine, how the joint moves and how much stress is applied across a joint can play a large role in how much pain you experience and how much you have to limit your activities. Proper strength and flexibility in the muscles surrounding the joint can optimize the movement of the joint and may reduce some of the rubbing that occurs between uneven joint surfaces. Your physical therapist will test your muscles to identify areas that need work and can guide you through a progressive program of exercises to address these issues.
As muscles get stronger and tissues regain their proper length and flexibility, learning to activate muscles at the right time and in the right order during a specific activity is essential. Even if your muscles are strong, the motor control of these muscles may not be adequate to properly perform a movement without putting excessive stress across a certain joint. As you learn to control and fire your muscles while performing motions such as going up stairs or running, you will experience less pain.
The ultimate goal of a physical therapy program is to help you get back to the activities you love and need to do throughout your life. While you may not be able to prevent every gout attack, you can help prevent long-term disability associated with joint injury and inactivity. Don’t let gout get in your way of a happier, healthier, and more active life. Schedule an appointment with a physical therapist at Evolve where they will empower you to make lifestyle changes to reduce your risk for another gout attack and help you get back to activities in the safest, most effective and quickest way possible.
Click here for more information about physical therapy for Gout
About EvolveNY-
Brooklyn's Premier Holistic Physical Therapy Clinics- There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
https://EvolveNY.com
Are Your Fingers Tingling? It May Be Carpal Tunnel Syndrome
Getting Control of Your Carpal Tunnel Syndrome with Physical Therapy: WHAT IS CARPAL TUNNEL SYNDROME? Have you been experiencing numbness, tingling, or burning in your palm, thumb, index or middle fingers? In the beginning maybe you would wake up with these symptoms and be able to relieve them quickly but now they are occurring more often during the day, especially after you’ve been using your hands for a while. The numbness might linger and eventually you start noticing some weakness in your hands. If this sounds familiar, you might be experiencing carpal tunnel syndrome (CTS).
Physical Therapy for Carpal Tunnel Syndrome
Getting Control of Your Carpal Tunnel Syndrome with Physical Therapy…
WHAT IS CARPAL TUNNEL SYNDROME?
Have you been experiencing numbness, tingling, or burning in your palm, thumb, index or middle fingers? In the beginning maybe you would wake up with these symptoms and be able to relieve them quickly but now they are occurring more often during the day, especially after you’ve been using your hands for a while. The numbness might linger and eventually you start noticing some weakness in your hands. If this sounds familiar, you might be experiencing carpal tunnel syndrome (CTS).
Carpal tunnel syndrome refers to a group of symptoms that are caused by pressure on the median nerve as it passes through the carpal tunnel of the wrist. The carpal tunnel is a narrow passageway on the palm side of the wrist created by a ligament called the transverse carpal ligament that crosses from left to right between several wrist bones. The median nerve and several tendons travel through and are protected by the carpal tunnel.
The median nerve arises from the neck region of the spinal cord and travels through the muscles and tissues of the upper arm and forearm, through the carpal tunnel and it’s branches travel into the hand. The median nerve supplies motor impulses to several forearm and hand muscles and transmits sensory information between the thumb, index, middle, and half the ring fingers, their corresponding palm areas, and the brain.
You can see why pressure on the median nerve as it travels through the carpal tunnel would cause numbness, tingling or burning in the first 3 (and sometimes part of the 4th) fingers. In fact many people find themselves shaking their hands out frequently to relieve these sensations. If the compression is prolonged or severe, it can interfere with the nerve’s ability to transmit motor signals to corresponding muscles and a person can notice weakness in their hands and grasp and more difficulty performing fine motor tasks such as typing, writing, or handling small objects.
WHO IS AT RISK FOR DEVELOPING CTS?
While nerves are pretty resilient against occasional pressure and compression, prolonged pressure can cause the types of symptoms we see with CTS. Because of the nature of this condition, repetitive forceful finger use, prolonged vibration through the hands, and extreme wrist positions can raise your risk of developing CTS. Data shows that women are more than three times more likely to develop CTS and that certain professionals such as assembly line workers, manufacturing, sewing, cleaning, and meatpacking workers develop CTS at higher rates. Even repetitive typing and keyboarding, if the wrists are angled less than optimally, can cause CTS.
CTS is also associated with certain health conditions in some people:
Trauma or injury to the wrist that causes inflammation such as a fracture or sprain
Diabetes
Overactive pituitary gland
Underactive thyroid gland
Rheumatoid arthritis or gout
Fluid retention during pregnancy or menopause
Hand or wrist deformities
HOW IS THIS CONDITION DIAGNOSED?
A thorough subjective exam is often adequate to diagnose CTS. Your physical therapist will ask you about the duration and nature of your symptoms and what kinds of activities you do in your job, for recreation and in your daily tasks. This information gives the physical therapist insight into potential underlying causes and helps rule out other conditions that may cause symptoms in the hand and fingers.
Once they have interviewed you, you can expect to undergo a physical exam to evaluate your strength, sensation and coordination of your affected hand and forearm. Your PT will likely also examine your neck and shoulder as the median nerve originates in the neck and at times conditions of the neck can mimic symptoms of CTS. They may also perform certain special tests to detect compression and irritation of the median nerve:
Phalen’s test: gently pressing the backs of your hands together to flex both wrists for one minute. Tingling or numbness in the fingers that occurs within 60s is suggestive of CTS
Tinel sign: your physical therapist may tap over the median nerve where it passes through the wrist. Tingling that results in the thumb, middle or index finger may indicate CTS
If you see a specialist physician such as a Neurologist, they may recommend specialized electrical and nerve function testing such as an electromyogram (EMG) to determine how well motor impulses are traveling through the nerve. A nerve conduction velocity test may also be utilized to assess how well the median nerve transmits sensory information. These tests can identify and assess severity of CTS. In some cases an x-ray or MRI may be ordered to assess for possible trauma or deformity in that area.
HOW CAN PHYSICAL THERAPY IMPROVE MY SYMPTOMS?
Physical therapy can be helpful in improving symptoms as a form of conservative care or as part of a post-surgical rehabilitation plan. Non-surgical treatments are typically recommended first and may include physical therapy, corticosteroid injections or non-steroidal anti-inflammatory medications prescribed by a physician, and splinting. If the condition is severe or does not respond to conservative treatment then surgical intervention may be recommended to create more space within the carpal tunnel to relieve the pressure on the median nerve.
A physical therapist will always create an individualized plan to meet your specific needs but generally aims to reduce your pain and help prevent surgery, increase your ability to be functional and active, and help you resume your normal work, home and leisure activities. If PT is recommended after CTS surgery then additional goals will include minimizing scar formation and restoring normal strength and range of motion.
Due to the nature of CTS, you can expect that education and activity modifications will be an important part of your custom physical therapy program. Understanding what specific activities and hand/wrist positions may have caused your symptoms to develop in the first place is an important step in improving symptoms and reducing the likelihood of recurrence. Modifying the tools you use, taking breaks, adjusting your workspace to allow for a more neutral wrist position and reducing the force that you put repetitively through your wrist and hands are just a few of the suggestions your PT may make to help prevent return or worsening of CTS.
If you start to notice any of these symptoms developing it is important to seek treatment early, however, much can still be done even if you’ve had these symptoms for a while. A physical therapist at Evolve is trained to help identity signs and symptoms of CTS and can recommend modifications you can make immediately to start improving your symptoms but perhaps more importantly, can prescribe a plan of treatments to help you recover the strength and sensation you have lost, reduce your pain and get you back to your regular activities with the confidence in knowing how to prevent carpal tunnel syndrome from returning.
Click here for more information about physical therapy for carpal tunnel syndrome
About EvolveNY-
Brooklyn's Premier Holistic Physical Therapy Clinics- There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
Healing Your Back May Be Easier Than You Think
Physical Therapy for Your Back- Is Your Back Bothering You? Call a Physical Therapist in Brooklyn Today! Are you looking for a way to relieve pain in your back? Do your back muscles feel weak? Is your back tight after sitting, standing or lifting all day at work? If this sounds familiar, you may need physical therapy for your back. Believe it or not, every movement you make with your arms, your legs, or your head translates some kind of stress or strain to the joints of the spine.
Physical Therapy for Your Back
Is Your Back Bothering You? Call a Physical Therapist in Brooklyn Today!
Are you looking for a way to relieve pain in your back? Do your back muscles feel weak? Is your back tight after sitting, standing or lifting all day at work? If this sounds familiar, you may need physical therapy for your back. Believe it or not, every movement you make with your arms, your legs, or your head translates some kind of stress or strain to the joints of the spine.
If you are bending and squatting down to pick up boxes all day but your hips are tight and glute muscles are weak, you may notice an annoying ache in your back. When your upper back is stiff and the muscles in the front of your chest are shortened from spending all day on your computer, your neck may be killing you after a day spent studying for exams. Finally, if you accidentally stepped off of the curb while reading a text message your lower back muscles might be spasming in response.
Whether these symptoms are new or chronic, mildly annoying or completely disruptive to your normal routines, physical therapy can help! Physical therapists are specially trained to get to the bottom of your back symptoms and get you on a program that creates long lasting results.
LET’S START BY LOOKING CLOSER AT YOUR BACK
When we talk about the back we are usually referring to the upper, middle and lower spine and the muscles on either side of it. The seven vertebrae that make up the neck, known as the cervical spine, the 12 vertebrae that make up the mid back, or thoracic spine, and the 5 vertebrae that make up the lower back, or lumbar spine, create a long canal that houses the spinal cord. The spinal cord is made up of a bundle of nerves that arise from the brainstem and leave through channels between the bones of the spine to innervate and carry movement and sensation information between the brain and the rest of the body. The broad and flat sacral bones sit beneath the last lumbar vertebrae and act as connectors between the pelvic bones and the spine. Beneath that, lies the coccyx or tailbone.
In between each vertebrae is an intervertebral disc. These discs transmit forces, act as shock absorbers and facilitate motion in the spine. Loss of fluid in the discs is responsible, in part, for why we tend to become shorter as we age. Sometimes the intervertebral discs can herniate, or rupture, and put pressure on the spinal cord or nerve roots causing localized or radiating pain, changes in strength and sensation in the arms or legs.
There are also many muscles that criss-cross the back. Some muscles are more superficial--closer to the skin--and often help in moving or positioning the arms. Intermediate layers of muscles act on the ribcage to help with respiratory function and deep layers of muscles help move the spine. While not technically part of the back, the abdominal muscles are also worth mentioning here as they are intimately connected to the fascial layers of the back and work together to help stabilize the lower spine.
GETTING TO THE ROOT OF YOUR BACK PROBLEMS
Now that you have a better understanding of the structures that make up the back, it’s important to understand that any of these anatomical structures may be involved in back symptoms. Whether you call it tightness, pain, discomfort, weakness or irritation, most back symptoms can be helped with conservative treatments like physical therapy but it starts with identifying the underlying cause(s).
When you schedule an evaluation with a physical therapist, the purpose is to understand when your symptoms started, what makes them better or worse, what might be causing them and what your goals are for working with a PT.
In some cases, a specific anatomical structure may be primarily to blame for your symptoms, such as the herniation of an intervertebral disc or a strain of a specific muscle but often times the underlying cause is due to faulty movement patterns or lack of strength and flexibility in other areas of the body. For example, if you aren’t able to raise your arm all the way overhead but you spend hours a day stacking items on high shelves at the grocery store, there is a good chance you are extending or arching your back further than you should to try and reach a little higher. Over time, this causes excess strain in the joints and muscles of the back and can lead to discomfort or pain.
Because back symptoms are often multifactorial, your physical therapist will be evaluating how you move your arms, legs and spine as much as he or she is examining the specific structures of the back.
HOW CAN PHYSICAL THERAPY HELP YOUR BACK?
Once the underlying causes have been pinpointed, it’s time to get to work. Physical therapy aims to give you immediate relief of your symptoms whenever possible, but most importantly, aims to address the underlying causes to reduce the likelihood they will return in the future. Here are some ways PTs will address your symptoms when you come in for a physical therapy treatment:
Reduce pain, inflammation and irritation: While completely eliminating your symptoms may take time, making you more comfortable in the meantime is an important first step in your rehabilitation. Applying ice or heat, ultrasound or electrical stimulation to the affected area can often give you some relief. Soft tissue mobilization or gentle joint mobilization may also be employed by your physical therapist to reduce tissue irritation.
Improve flexibility: Each activity you perform throughout your day requires your joints to move through a certain range of motion. When a joint lacks the flexibility needed to perform the movement optimally, extra stress and strain is translated to other parts of the body. Your back PT program may include stretching, myofascial release techniques, joint mobilization and mobility exercises to improve flexibility in the back itself but also in other areas of the body such as the ankles, hips, and shoulders.
Build up your strength: Now that we’ve improved your flexibility, it is important to strengthen the muscles around your spine and other joints. Just as lack of flexibility around joints of the arms and legs can lead to pain or tightness in the back, lack of strength and stability can too. You will learn exercises to help strengthen the muscles around the back and abdomen to properly stabilize the spine and also in the arms and legs to minimize excess strain transfer to the back. Having good strength throughout the body allows stress to be distributed across multiple joints and helps to prevent injury and irritation in the future.
Optimize your movement: Reducing inflammation and pain and balancing strength and flexibility across the body are only the first steps to treating your back. Many of the tasks we do throughout the day require complex, multi joint movements. Just think about how many joints are moving and muscles are working when you reach down to lift a box off the floor or serve a tennis ball at the beginning of a point. Learning proper biomechanics and enhancing the neuromuscular control of joints and muscles is an essential component of healing and preventing back injuries. Physical therapists are movement experts and through analyzing your movements, can guide you in improving how you move and train your muscles to perform those movements in the safest and most effective way possible.
While back symptoms can be disruptive to your daily life, conservative treatments such as physical therapy are often highly effective. Physical therapists can identify the myriad of factors contributing to your specific back symptoms and provide you with a rehabilitation program to improve them now and help prevent them in the future. A physical therapist at Evolve can help you get on the road to healing your back.
Click here for more information about physical therapy for upper and lower back pain
About EvolveNY-
Brooklyn's Premier Holistic Physical Therapy Clinics- There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
https://EvolveNY.com
Are You Suffering From a Knee Injury?
Knee Physical Therapy Can Get You Back on Your Feet- The knee is a hinge joint that flexes and extends. While it has fairly simple mechanics, it is responsible for creating and absorbing forces that come from walking, running, jumping, going up and down stairs, getting on and off the floor and much more. Because it is involved in so many of the movements we perform throughout our day it is susceptible to injury and discomfort caused by long term accumulation of stress or a sudden uncontrolled force. Whether you are experiencing new knee pain or have been living with it for some time, a physical therapist can help get to the root cause and improve your knee symptoms...
Knee Physical Therapy Can Get You Back on Your Feet
The knee is a hinge joint that flexes and extends. While it has fairly simple mechanics, it is responsible for creating and absorbing forces that come from walking, running, jumping, going up and down stairs, getting on and off the floor and much more. Because it is involved in so many of the movements we perform throughout our day it is susceptible to injury and discomfort caused by long term accumulation of stress or a sudden uncontrolled force. Whether you are experiencing new knee pain or have been living with it for some time, a physical therapist can help get to the root cause and improve your knee symptoms.
LET’S EXAMINE THE KNEE MORE CLOSELY
The knee joint is where the cartilage-covered ends of the thigh bone (femur) and lower leg bone (tibia) meet. The patella, also known as the kneecap, sits at the front of the joint within the tendon of the large quadriceps muscle and acts as a fulcrum to increase the power of these large thigh muscles. Two moon-shaped menisci cushion the joint on the medial and lateral sides.
Four main ligaments provide stability to this knee joint. The medial collateral ligament (MCL) runs up and down on the inside of the knee to prevent the knee from buckling inward. The lateral collateral ligament (LCL) runs up and down on the outside of the knee to prevent the joint from buckling outward. The anterior cruciate ligament (ACL) runs through the center of the joint from the tibia to the femur and primarily restrains anterior translation of either bone though acts to restrain excess movement in other planes as well. Finally, the posterior collateral ligament (PCL) similarly runs between the tibia and femur and primarily restrains posterior translation of either bone.
The hamstring muscles and calf muscle in the back attach near either side of the knee joint to help flex the knee while the quadriceps muscles extend the joint and run across the front of the knee attaching below it. The adductor muscle group which attaches near the groin runs down the inside of the leg and attaches above and below the knee.
WHAT KNEE CONDITIONS CAN PHYSICAL THERAPY TREAT?
Muscle Strain: When overstretched, overused or contracted against a sudden load, a muscle strain can occur as muscle fibers or the musculotendinous junction are torn or injured. A muscle strain in the hamstring or calf muscles in the back or the quadriceps muscles in the front can cause pain near the knee joint. Muscle strains can range from mild to severe depending on how much of the muscle is affected. You may experience pain, swelling, tenderness or bruising with pain during muscle contraction.
Ligament Sprains/Tears: ligaments are bands of collagen tissue that support bones, joints and organs. As outlined above there are four main ligaments in the knee joint. Because the primary function of ligaments is to provide passive stabilization to the area, loss of stability can range from mild to severe with a ligament sprain depending on how many fibers are torn.
MCL Sprain/Tear: An injury to this ligament often occurs during sudden bending, twisting or direction changes or when the outside of the knee is hit such as during a football tackle. Initially pain and tenderness on the inside of the knee may be felt and swelling and stiffness may develop later on. If the sprain is severe enough the knee joint may eventually feel unstable.
LCL Sprain/Tear: Sharp turns with a planted foot, sudden hyperextension of the joint, or a hit on the inside of the knee can all cause a sprain to the LCL. Pain, swelling and tenderness on the outside of the knee are common. Depending on the severity you may also experience locking or catching and possibly giving way during movement.
ACL Sprain/Tear: This ligament can be injured from a direct hit to the knee such as during a soccer game or if the upper leg suddenly twists while the foot is planted. Sometimes landing on a hyperextended knee or stopping momentum suddenly can also injure the ACL. A sharp intense pain and an audible pop may occur at the moment of injury. You may be unable to support any weight through the joint immediately and swelling typically develops shortly after.
PCL Sprain/Tear: Injury to the PCL most often occurs when a sudden force shifts the lower leg bone backwards under the upper thigh bone. Knee injuries that damage the PCL often injure other ligaments or cartilage in the knee and sometimes a small fragment of bone can break free. Swelling and stiffness are common with this injury. Pain may be felt inside the knee joint or at the back of the knee and made worse with squatting, running, or climbing stairs.
Iliotibial (IT) Band Syndrome: The IT Band is a thick band of tissue that runs along the outside of the leg from the pelvis to the knee. Irritation and inflammation around this band can occur from repetitive straightening and bending during activities such as running and cycling. Stabbing or stinging pain felt along the outside of the knee is often felt when going from a sitting to a standing position or following continuous activities such as walking or stair climbing.
Tendinopathies: Tendons are the thick, fibrous bands or cords that attach muscle fibers to bones. Pain felt outside of a joint at the end of a muscle which is exacerbated by movement may be tendonitis or tendinopathy. In the knee, this most commonly occurs at the hamstring tendons where they attach on either side of the knee posteriorly and in the patellar tendon below the patella. The most common cause of inflammation and irritation in the tendon is repetitive overuse. Often biomechanical or movement errors, muscle strength and length asymmetries or insufficiencies are an underlying cause. Pain is usually described as a dull ache that can interfere with your activities. Tenderness, mild swelling and general weakness may also be present.
Patellofemoral Pain Syndrome: This condition refers to pain at the front of the knee felt under or around the patella. It is worse with activity and sometimes after sitting for long periods of time with a bent knee. It is a common cause of knee pain and often occurs in response to an increase in activity that occurs faster than the tissues of the knee can adapt.
Osteoarthritis: Arthritis can occur in any joint. In the knee, osteoarthritis refers to breakdown of the cartilage that covers the ends of each bony surface and a loss of synovial fluid that lubricates the joint. This results in rubbing of bony surfaces together causing pain and stiffness. In severe cases a total knee arthroplasty (replacement) may be performed by a surgeon. While physical therapists cannot reverse the OA itself, physical therapy has proven to be an effective treatment modality for arthritis. Restoration of optimal joint movement, addressing biomechanics and movement pattern inefficiencies, maximizing muscle strength and education on possible activity modifications are all helpful.
Meniscal Tear: Tears of either meniscus can be “acute”, meaning it occurred as the result of a sudden injury or “degenerative”, meaning it occurred over time. Acute injury to these cartilaginous discs often occurs when the upper leg is twisted or turned while the knee is bent and the foot is planted. Symptoms of a meniscal tear include a sharp intense pain in the knee and difficulty walking or going up and down stairs. If this is an acute injury a pop or tearing sensation may occur and swelling typically develops within about 24 hours. Some meniscus tears can cause a locking or catching sensation that restricts fully bending or straightening the knee.
HOW WILL YOUR PHYSICAL THERAPIST TREAT YOUR LEG?
Initially your PT will assess your knee to determine the cause and contributing factors to your symptoms and then will begin a customized treatment plan to get you back on your feet.
If you are being treated for an acute injury such as a tear or strain, your physical therapist will educate you on how to protect these newly healing tissues. Treatment may include compression or bracing, offloading the injured area through crutches, modalities such as ice, ultrasound or electrical stimulation to reduce pain and swelling and activity modification.
In well-healed tissues, chronic injuries like tendinopathy or IT band syndrome, your physical therapy program will focus not only on reducing or eliminating localized symptoms but on addressing factors that contributed to the onset of the symptoms. Often injuries or pain in the knee are caused by repeating faulty movement patterns or having an imbalance of muscle strength and length to carry out a task such as walking, running, cutting, or jumping optimally and with good mechanics.
While some knee injuries may require intervention by a doctor or surgeon, a physical therapist should always be a primary member of your care team. A physical therapist at Evolve can help you get on the road to recovery. Our therapists do not just treat symptoms, but we get to the root of the cause. We strive to enable our patients to live pain free, and prevent the recurrence of related issues. Click here for more information about knee physical therapy .
About EvolveNY-
Brooklyn's Premier Holistic Physical Therapy Clinics-
There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better! First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
Experiencing Discomfort in Your Legs?
HOW CAN A PHYSICAL THERAPIST HELP YOUR LEG PAIN? Sprains, strains, pulled muscles, broken bones, fractures and sciatica are just some of the reasons a person may visit a physical therapist for their leg. Sometimes it can be difficult to determine the cause of your pain or discomfort but a physical therapist is trained to evaluate the myriad contributing factors to identify the most likely causes and craft a plan of action to improve your symptoms...
What are some of the injuries of the leg that Physical Therapy can treat?
Sprains, strains, pulled muscles, broken bones, fractures and sciatica are just some of the reasons a person may visit a physical therapist for their leg. Sometimes it can be difficult to determine the cause of your pain or discomfort but a physical therapist is trained to evaluate the myriad contributing factors to identify the most likely causes and craft a plan of action to improve your symptoms.
WHAT LEG CONDITIONS CAN A PHYSICAL THERAPIST TREAT?
Sciatica: Sciatica refers to pain, burning, tingling, cramping, numbness and sometimes weakness that often begins in the buttock and travels down the back of the leg. It is caused by compression or irritation of the sciatic nerve that originates in the low back and travels down the posterior leg. With severe or prolonged compression or irritation muscle weakness can also occur. Your physical therapist will be assessing for a number of causes including disc herniations, misalignment of the pelvis, tightness in the hip or buttock muscles, narrowing of the spine or biomechanical problems before they begin treating you.
Muscle Strain: Muscles are made up of bundles of muscle fibers aligned in specific patterns. When these fibers contract they shorten the muscle and pull on the bones they attach to creating movement and strength. At either end of these fibers is a strong band of tissue called the tendon which connects the fibers to the bone. When overstretched, overused or contracted against a sudden load, a muscle strain can occur as muscle fibers or the musculotendinous junction are torn or injured.
Grade I strain (mild): very few muscle fibers are injured. Pain typically occurs the next day but no swelling or bruising is observed. Pain may be felt when the affected muscle is strongly contracted or stretched at its end range.
Grade II strain (moderate): many (but not all) fibers are injured resulting in stiffness, loss of flexibility and loss of strength. Pain is felt both during contraction of the muscle and during stretching. Swelling and bruising over the injured area is common.
Grade III strain (severe): all fibers of the muscle are completely torn or the muscle belly has detached from it’s tendon. Severe pain is often felt upon injury and heavy swelling and bruising will develop. Range of motion may be either significantly reduced due to pain or excessive because the muscle is no longer limiting it. This muscle will generally be unable to produce any force due to the severe disruption in the fibers.
Ligament Sprains: ligaments are bands of collagen tissue that support bones, joints and organs. In the leg the most common ligament sprains occur at the knee and ankle. A sprain typically occurs when these inelastic fibers are stretched beyond their capacity such as when you twist your knee or roll your ankle. Because the primary function of ligaments is to provide passive stabilization to the area, loss of stability can range from mild to severe with a ligament sprain.
Grade I (mild): microscopic damage has occurred to the ligament but only mild local tenderness and minimal bruising/swelling is noted without compromising joint stability. Typically takes 2-3 weeks to heal.
Grade II (moderate): partial tear/rupture of the ligament. Obvious swelling and tenderness noted over the injured ligament but joint instability is either minimal or absent. May require up to 6 weeks to heal.
Grade III (severe): complete rupture of the ligament with severe swelling and tenderness. This injury may be difficult to distinguish from a fracture initially. Instability of the joint is noticeable due to the severity of the rupture. Prolonged time to heal is frequent and may require surgery to repair.
Tendinopathy: Tendons are the thick, fibrous bands or cords that attach muscle fibers to bones. Pain felt outside of a joint at the end of a muscle which is exacerbated by movement may be tendonitis or tendinopathy. The most common cause of inflammation and irritation in the tendon is repetitive overuse. Often biomechanical or movement errors, muscle strength and length asymmetries or insufficiencies are an underlying cause. Pain is usually described as a dull ache that can interfere with your activities. Tenderness, mild swelling and general weakness may also be present. Patellar tendinopathy, achilles tendinopathy and hip flexor tendinopathy are examples of tendon irritation that may occur in the leg.
Muscle contusion: muscle contusions (bruises) are a common cause of injury in contact sports. Minor contusions typically heal quickly with little disruption to sports or daily life. A direct or repeated blow to the muscle can cause a severe contusion, however, which causes deep tissue damage to the muscle fibers and connective tissue and can take a long time to heal. Swelling, stiffness, weakness, localized bruising and pain are common. Sometimes a pool of blood called a hematoma can form over the area. Severe muscle contusions should always be evaluated by a health professional as there is a right and a wrong way to treat these injuries.
HOW WILL YOUR PHYSICAL THERAPIST TREAT YOUR LEG?
As you can see, leg injuries can vary widely and at times symptoms may even be referred from another area such as your back. Initially your PT will assess your leg to determine the cause and contributing factors to your symptoms and then will begin a customized treatment plan to get you back on your feet.
If you are being treated for an acute injury such as a sprain or strain, your physical therapist will educate you on how to protect these newly healing tissues. Treatment may include compression or bracing, offloading the injured area through crutches, modalities such as ice, ultrasound or electrical stimulation to reduce pain and swelling and activity modification.
In well-healed tissues, chronic injuries like tendinopathy or referred conditions like sciatica, your physical therapy program will focus not only on reducing or eliminating localized symptoms but on addressing factors that contributed to the onset of the symptoms. Often injuries or pain in the leg are caused by repeating faulty movement patterns or having an imbalance of muscle strength and length to carry out a task such as running, cutting, or jumping optimally and with good mechanics.
While some leg injuries may require intervention by a doctor or surgeon, a physical therapist should always be a primary member of your care team. A physical therapist at Evolve can help you get on the road to recovery. Our therapists do not just treat symptoms, but we get to the root of the cause. We strive to enable our patients to live pain free, and to prevent the recurrence of related issues.
Click here to find out more about leg physical therapy in Brooklyn.
About EvolveNY-
Brooklyn's Premier Holistic Physical Therapy Clinics- There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better! First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
https://EvolveNY.com
HIP INJURY GETTING IN YOUR WAY?
Physical Therapy for the Hip- HIP PAIN AND INJURY GETTING IN YOUR WAY? The hip joint is a ball and socket joint where the top of the femur meets the pelvis. The mechanics of this joint allow for a great deal of movement of the leg but requires the appropriate balance between mobility and stability to reduce likelihood of injuries. True hip joint pain is felt deep in the groin area but many other conditions involving muscles, tendons or nerves surrounding the hip may be felt above, below and to the side of this area...
Physical Therapy for the Hip
HIP PAIN AND INJURY GETTING IN YOUR WAY?
The hip joint is a ball and socket joint where the top of the femur meets the pelvis. The mechanics of this joint allow for a great deal of movement of the leg but requires the appropriate balance between mobility and stability to reduce likelihood of injuries. True hip joint pain is felt deep in the groin area but many other conditions involving muscles, tendons or nerves surrounding the hip may be felt above, below and to the side of this area.
WHAT HIP CONDITIONS CAN A PHYSICAL THERAPIST TREAT?
Bursitis: Bursa are small sacks of fluid that act as cushions over a bony area. The most common area for bursitis in the hip is on the greater trochanter of the hip on the outside of the upper leg. Bursa can become inflamed or irritated with repetitive friction usually caused by activities such as long distance walking on uneven surfaces or on uneven legs, running up hills or even by a direct trauma such as falling on the hip. Bursitis can cause pain and irritation when lying on the hip, lifting the leg, climbing stairs or walking. Physical therapy can help reduce inflammation and pain and address contributing factors such as muscle weakness, leg length discrepancies or movement pattern errors to resolve symptoms and limit recurrence.
Labral Tear: An injury to the band of cartilage that lines the outside of the hip joint is called a labral tear. A tear in this area can occur from a trauma such as a fall or car accident but is more often the result of repetitive stress and strain during activities such as deep squatting, cutting and twisting. It is more likely to occur in the presence of bony abnormalities in the hip joint (hip impingement). Typical symptoms include dull pain felt deep in the groin that can be sharp with low squatting, clicking or catching of the hip with movement, pain and stiffness that is worse after prolonged sitting or walking and stiffness or muscle weakness. This cartilaginous ring is not capable of healing on its own so some people may opt for surgery. Others can achieve a satisfactory level of symptom reduction and return to activity with physical therapy to optimize muscle strength and length and address movement patterns.
Osteoarthritis: Arthritis can occur in any joint. In the hip, osteoarthritis refers to breakdown of the cartilage that covers the femoral head (ball of the hip) and lines the acetabulum (socket of the pelvis) and a loss of synovial fluid that lubricates the joint. This results in rubbing of bony surfaces together causing pain and stiffness. In severe cases a total hip arthroplasty (replacement) may be performed by a surgeon. While physical therapists cannot reverse the OA itself, arthrtitis physical therapy has proven an effective treatment modality for arthritis. Restoration of optimal joint movement, addressing biomechanics and movement pattern inefficiencies, maximizing muscle strength and education on possible activity modifications are all helpful.
Muscle Strain: Muscles are made up of bundles of muscle fibers aligned in specific patterns. When these fibers contract they shorten the muscle and pull on the bones they attach to creating movement and strength. At either end of these fibers is a strong band of tissue called the tendon which connects the fibers to the bone. When overstretched, overused or contracted against a sudden load, a muscle strain can occur as muscle fibers or the musculotendinous junction are torn or injured.
Grade I strain (mild): very few muscle fibers are injured. Pain typically occurs the next day but no swelling or bruising is observed. Pain may be felt when the affected muscle is strongly contracted or stretched at its end range.
Grade II strain (moderate): many (but not all) fibers are injured resulting in stiffness, loss of flexibility and loss of strength. Pain is felt both during contraction of the muscle and stretching. Swelling and bruising over the injured area is common.
Grade III strain (severe): all fibers of the muscle are completely torn or the muscle belly has detached from it’s tendon. Severe pain is often felt upon injury and heavy swelling and bruising will develop. Range of motion may be either significantly reduced due to pain or excessive because the muscle is no longer limiting it. This muscle will generally be unable to produce any force due to the severe disruption in the fibers
Peripheral Nerve Entrapment: This condition refers to compression of a nerve as it passes through structures around the hip. Depending on the location and severity you may experience radiating pain or burning sensation, numbness or tingling or muscle weakness. Manual therapy techniques such as soft tissue mobilization or stretching may help reduce compression. Taping to offload the area may also help. Your physical therapist may also prescribe strengthening exercises to ensure surrounding musculature can support the affected area while minimizing compression.
Tendinopathy: Tendons are the thick, fibrous bands or cords that attach muscle fibers to bones. Pain felt outside of a joint at the end of a muscle which is exacerbated by movement may be tendinopathy. The most common cause of inflammation and irritation in the tendon is repetitive overuse. Often biomechanical or movement errors, muscle strength and length asymmetries or insufficiencies are an underlying cause. Pain is usually described as a dull ache that can interfere with your activities. Tenderness, mild swelling and general weakness may also be present. Patellar tendinopathy, achilles tendinopathy and hip flexor tendinopathy are examples of tendon irritation that may occur in the leg.
LET US HELP YOU GET ON THE ROAD TO HEALING
While a physical therapist cannot repair the labrum or reverse osteoarthritic changes in the joint, physical therapy is an excellent treatment option for acute and chronic hip pain and injuries. Your body was meant to move and whether you are looking for help rehabilitating after surgery or conservative treatment for discomfort that is keeping you from participating in home, work or recreational activities, physical therapy should be at the top of your list. Through a thorough assessment and evaluation, a physical therapist at Evolve can get to the root of your problem and develop a plan of care that will not only treat your symptoms but enable you to stay active for as long as you like by preventing the recurrence of related issues.
Click here for more information about hip physical therapy in Brooklyn
About EvolveNY-
Brooklyn's Premier Holistic Physical Therapy Clinics- There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
https://EvolveNY.com
Physical Therapy for Foot Pain and Injury
Physical Therapy for Foot Pain and Injury- IS PAIN IN THE FOOT GETTING YOU DOWN? Feet, the literal foundation of our bodies. The important role our feet play in our daily activities cannot be underestimated. This is why, when you have pain or injury in one or both feet, your day to day life can be significantly affected. While some injuries to the foot require surgery to correct, many can be addressed through the care of a physical therapist. Whether you are recovering from surgery or looking for a more conservative approach, a physical therapist is an important member of your care team and can work with you to get you back to walking, running and dancing your way through life. This article will help you to understand the causes, symptoms and possible interventions that you can expect during a physical therapy treatment…
Physical Therapy for Foot Pain and Injury
IS PAIN IN THE FOOT GETTING YOU DOWN?
Feet, the literal foundation of our bodies. The important role our feet play in our daily activities cannot be underestimated. This is why, when you have pain or injury in one or both feet, your day to day life can be significantly affected. While some injuries to the foot require surgery to correct, many can be addressed through the care of a physical therapist. Whether you are recovering from surgery or looking for a more conservative approach, a physical therapist is an important member of your care team and can work with you to get you back to walking, running and dancing your way through life. This article will help you to understand the causes, symptoms and possible interventions that you can expect during a physical therapy treatment.
LET’S GET A BETTER UNDERSTANDING OF THE FOOT AND HOW IT FUNCTIONS:
Each foot is made up of 28 individual bones that can be divided functionally into a hindfoot, a midfoot and a forefoot. Numerous ligaments intertwine between bones to create shape and connection. Nearly 30 muscles--some originating from the lower leg and others within the foot itself--work together to create the delicate balance of mobility and stability in this area of the body.
Another star player in the foot is the plantar fascia. A thick layer of tissue, it runs from the heel of the foot to the ball of the foot. When standing, the plantar fascia helps to create the arch of the foot. While walking and moving, it assists in altering the position of the foot as you move through a normal gait cycle and acts as a shock absorber.
In addition to these structures we can’t forget the nerves in the skin and joints of the feet that act as vital purveyors of information as you stand, walk, run and jump. We rely heavily on the accuracy of sensory information gleaned from these receptors to maintain our balance and coordinate movements throughout the body.
What is important to understand about the foot is that changes in the anatomical structure of the foot, strength of the muscles, stability of the ligaments and flexibility of the tissues as well as alterations in the motor control and biomechanics of the foot can impair the function and balance of each joint and body part above it. Even if your primary symptoms are not in your feet, your physical therapist will be observing how your feet function and move because problems in the foundation of your body can have widespread implications.
WHAT MIGHT BE THE CAUSE OF YOUR SYMPTOMS?
Disorders of the foot come in many varieties. Some people are born with conditions that alter the normal anatomy of the foot such as Pes Planus (flat foot), Pes Cavus (high arches), or Talipes Equinovarus (clubfoot). These conditions may require surgical intervention, bracing or special footwear throughout an individual’s life.
Some instances of foot pain are caused by asymmetries or imbalances in muscle strength or flexibility, motor control and movement patterns of the lower body. In these cases, your physical therapist may prescribe a series of exercises to improve strength and flexibility. They may employ modalities such as ultrasound or ice to address inflammation or pain and manual therapy techniques such as joint mobilization, active release therapy(ART), or soft tissue mobilization.
Some other conditions of the foot that would benefit from the assessment and treatment of a skilled physical therapist are listed here:
Plantar Fasciitis: Inflammation and microtears can occur in this thick band of tissue causing pain in the heel, along the arch of the foot or near the ball of the foot. Oftentimes this pain is felt during the first few steps out of bed in the morning, after prolonged standing, during intense activity such as running or when walking barefoot or in shoes with poor support. While this condition may initially make it difficult to participate in your usual standing, walking or running routines, it often responds very well to physical therapy interventions aimed at reducing inflammation and promoting tissue healing, restoring optimal mobility at the foot and ankle joints, offloading the plantar fascia and strengthening surrounding muscles.
Turf Toe: Turf toe is the common name for a sprain of the metatarsophalangeal joint (MTP) of the first toe--where the big toe meets the foot. This is often a sports-related injury that occurs when the toe is hyperextended past its normal range of motion. In rare cases surgery may be required. Pain, swelling, and bruising over this area is common in the acute stage. Initially your physical therapist will educate you on how to protect the joint to allow healing to begin while applying ice or other modalities to help manage pain and swelling. When appropriate your PT will prescribe a progressive exercise program to restore normal strength and flexibility and build tolerance to loading through the joint.
Bunion: A bunion (hallux valgus) is a bony bump that develops on the inside of the foot at the base of the big toe. Oftentimes the big toe is no longer straight but instead deviates toward the other toes. Inflammation and swelling can occur in the area of the bunion and that area of the foot can become stiff and painful. Discomfort during walking or running and difficulty with the fit of shoes can occur over time. Bunions may be managed conservatively or when severe, surgically. In either case your physical therapist can recommend orthotics, footwear or toe separators to relieve discomfort and prevent worsening. They may prescribe range of motion exercises and strengthening to maximize foot biomechanics and provide hands on manual therapy if indicated.
Fractures: Fractures can occur traumatically or in response to chronic overload such as in the case of a stress fracture in a marathon runner. Whether managed surgically or conservatively, you will likely undergo a period of modified weight bearing to allow bone healing. Once appropriate, your physical therapist will employ many of the techniques outlined above to address any pain or stiffness that has developed, restore optimal strength and biomechanics of the foot and progress you back to normal walking, running and athletic events.
While foot pain or injury can be disruptive to your daily life, a physical therapist at Evolve can help you get on the road to recovery. Our therapists understand the importance that being able to stand, walk and participate in sports and leisure activities has in your life and we strive to enable our patients to live pain free, and prevent recurrence of the injuries.
Are you or someone you know experiencing foot pain? Call Evolve Physical Therapy in Brooklyn today to make an appointment. Our physical therapists will work with you to reduce the risk of complications, and help you get back to living your life to the fullest. Call- 1-718-258-3300 or visit- https://evolveny.com/physical-therapy/foot-physical-therapy-brooklyn
About EvolveNY-
Brooklyn's Premier Holistic Physical Therapy Clinics-
There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
https://EvolveNY.com
Elbow Issues Got You Down?
Physical Therapy for the Elbow- The elbow joint plays a critical role in connecting the mobile shoulder joint with the incredibly functional wrist and hands. Injuries to the elbow can interfere with your ability to play sports, to work, to do activities around the house and even to feed yourself. Whether your elbow injury is brand new or has been bothering your for quite a while, a physical therapist can perform an examination and apply physical therapy techniques to reduce your symptoms and get you back to your daily activities.This article will help you to understand the causes, symptoms and possible interventions that you can expect during a physical therapy treatment.
Physical Therapy for the Elbow: Elbow Discomfort Reducing Your Quality of Life?
The elbow joint plays a critical role in connecting the mobile shoulder joint with the incredibly functional wrist and hands. Injuries to the elbow can interfere with your ability to play sports, to work, to do activities around the house and even to feed yourself. Whether your elbow injury is brand new or has been bothering your for quite a while, a physical therapist can perform an examination and apply physical therapy techniques to reduce your symptoms and get you back to your daily activities.This article will help you to understand the causes, symptoms and possible interventions that you can expect during a physical therapy treatment.
LET’S GET TO KNOW THE ELBOW A BIT BETTER:
Most people know the elbow joint as a flexor and extensor of the arm and it certainly does this very well. The elbow joint also does what is called pronation and supination which rotate the forearm to translate the hand from a palm up to a palm down position and back. As you can see, the elbow joint plays a critical role in positioning your hands for functional tasks. This hinged joint is made up of the humerus or upper arm bone and the radius and ulna, the two bones of the forearm. Many ligaments stretch between the bones to connect and support them and tendons--the connective tissue end of a muscle--travel from the shoulder, wrist and hand to anchor near this joint. If you think about how many times in a day, an hour, or even a minute you bend or straighten your elbow or rotate your forearm up or down, you can see how this area of the body could experience some stress or strain.
WHAT MIGHT BE THE CAUSE OF YOUR ELBOW SYMPTOMS?
Tennis Elbow (Lateral Epicondylitis): Pain, burning or aching at the lateral (outside) elbow and forearm, sometimes extending down toward the wrist may be a condition called lateral epicondylitis. A result of strain or stress on the muscles and tendons that attach on the outer elbow, its often caused by repetitive motions of the wrist extensors in conjunction with impaired movement patterns and biomechanics, muscle length, strength and flexibility impairments. Left untreated, this condition can become painful even at rest and can lead to grip weakness over time.
Golfer’s Elbow (Medial Epicondylitis): Pain, burning or aching at the medial (inside) of the elbow and extending down toward the wrist is characteristic of medial epicondylitis. Symptoms may initially be present only during activities requiring repetitive wrist flexion like serving a tennis ball, hitting a golf ball, carrying a heavy suitcase or using certain hand tools but can eventually become symptomatic even at rest. Muscle strength or length impairments, movement pattern inefficiencies and biomechanical errors often contribute to this condition.
Olecranon Bursitis: The olecranon bursa is a small fluid-filled sac that covers the bony tip of the elbow (olecranon process) to help cushion it. When irritated or inflamed it can fill with extra fluid causing swelling of the back of the elbow. Some people will experience pain when they place their elbow on a firm surface or repeatedly bend it and on occasion the bursa can become infected causing warmth and redness in the area. This condition can occur from a hard fall on the elbow such as during a sporting event, as a result of spending prolonged periods of time resting the elbow on a hard surface such as a desk and is more common in certain occupations such as plumbing, gardening and mechanic work. It may also be more common in certain autoimmune conditions.
Cubital Tunnel Syndrome: The ulnar nerve is one of the three main nerves in the arm and travels from the neck, down the arm and to the hand. On it’s way, it passes through the inside bony part of the elbow called the cubital tunnel where it can sometimes experience compression. If you’ve ever hit your “funny bone” you know right where this spot is located. Signs of compression include numbness, tingling or loss of coordination in the ring and little fingers. In cases of severe compression muscle wasting or grip weakness can occur. Sometimes the cause is unknown. Other times it can be caused by arthritis, bone spurs, previous fractures or dislocations and sometimes by repeated bending of the elbow.
Elbow Ligament Injuries: Ligaments are bands of tissue that help hold bones, joints and organs in place. Many ligaments criss cross and surround the elbow joint and are vital to maintaining the stability and function of the joint. Injuries to the ligaments might occur as a result of repetitive strain, for example at the ulnar collateral ligament in baseball pitchers. In other cases, a ligament may be injured during an elbow dislocation when a person falls on an outstretched arm. Though these ligaments are quite resilient and persistent elbow instability is uncommon, physical therapy may be helpful in restoring normal motion and function soon after injury.
HOW WILL YOUR PHYSICAL THERAPIST TREAT YOUR ELBOW?
The first visit with your physical therapist will focus on assessing the elbow. Interviewing you about your symptoms and examining the arm will help your physical therapist to determine the most likely cause of your symptoms and to identify contributing factors such as strength asymmetries, range of motion deficits, tissue mobility problems or biomechanical errors. If you have recently had surgery on your elbow he or she may initiate care based on a post-surgical protocol assigned by your surgeon.
In the first week or so after an injury you can expect your elbow physical therapy treatment may include modalities such as ice, ultrasound or electrical stimulation to manage pain and swelling, education on your injury and any necessary activity modifications, gentle manual techniques such as passive range of motion and possibly taping or bracing to protect the injured area and allow the body’s healing process to proceed. As healing continues you may begin to perform a progressive exercise program to help strengthen the surrounding muscles and normalize muscle length. Your PT may apply manual therapy techniques such as soft tissue or joint mobilizations to restore normal motion. You can also expect to perform activities and exercises to prepare your body to return to it’s previous level of activity with special attention on correcting any movement asymmetries or motor control issues that may have contributed to the injury.
While some elbow injuries may require intervention by a doctor or surgeon, a physical therapist should always be a primary member of your care team. A physical therapist at Evolve can help you get on the road to recovery. Our therapists do not just treat symptoms, but we get to the root of the cause. We strive to enable our patients to live pain free, and prevent the recurrence of related issues
Are you or someone you know experiencing elbow pain? Call Evolve Physical Therapy in Brooklyn today to make an appointment. Our physical therapists will work with you to reduce the risk of complications, and help you get back to living your life to the fullest. Call- 1-718-258-3300 or visit- https://evolveny.com/physical-therapy/elbow-physical-therapy-brooklyn
About EvolveNY-
Brooklyn's Premier Holistic Physical Therapy Clinics-
There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
https://EvolveNY.com
FSA, “USE IT OR USE IT” RULE CANCELLED ?
FSA, “USE IT OR USE IT” RULE CANCELLED? Whats an FSA? FSAs, also commonly known as Medical FSA’s or Healthcare FSA’s, allow employees to stash away up to $2,750 for each qualifying account of pre taxed earnings for eligible health and wellness expenses that insurance doesn't cover. Some of the most popular expense usage are deductibles, copayments/coinsurance, vision care, Physical Therapy, and over-the-counter medicines or equipment.
FSA, “USE IT OR USE IT” RULE CANCELLED ?
It's that time of the year again, where we all scramble to gather our receipts to close out the tax year, schedule our last minute appointments before our health plans renew or change, and if you have a Flexible Spending Account (FSA) using your remaining pre-tax saving balance before its forfeited, can feel like a mad dash to beat the clock before your carriage (like cinderella) turns into a pumpkin.
Whats an FSA?
FSAs, also commonly known as Medical FSA’s or Healthcare FSA’s, allow employees to stash away up to $2,750 for each qualifying account of pre taxed earnings for eligible health and wellness expenses that insurance doesn't cover. Some of the most popular expense usage are deductibles, copayments/coinsurance, vision care, Physical Therapy, and over-the-counter medicines or equipment.
How do FSA’s work?
Under normal terms and circumstances, FSA accounts typically need to be spent and depleted by December 31st. If the account holder doesn’t use up all of the money in their account, they can roll over up to $550 to the next year, or spend it during a two-and-a-half-month grace period- depending on their employer. This leads many people in haste to spend down their accounts by stocking up on extra unneeded Advil, sunscreen, and other generic needs on amazon in excess just so they don't lose out. The rest of Americans forfeit an estimated 400 million per year.
What changes did the US Treasury make?
Well, there is good news for some! Regardless of which type of FSA you have, new legislation signed into law late last year allows you to roll over any unused funds from 2021 to 2022 for use at any time next year- if your company opts in. This is also applied to unused 2020 FSA money, which could be carried over into 2021. This provides 12 additional months for account holders to utilize their funds more intentionally and sensibly.
The best next steps ?
This is the time to find out if your employer opted in for this extension. Whether your employer opted in or not, don't be so quick to bring 2021 to a close without maximizing your health benefits. Now is the time to take advantage of any unused insurance benefits. Click Here to learn more about what other health benefits you can be losing out on.
Using all available benefits to complete any outstanding treatment, preventive or maintenance Physical Therapy sessions is one of the best ways to take a value added approach when considering how best to utilize your FSA funds. Even if you don’t have any immediate pain or issues, you and your family should always have treatment sessions and screenings periodically, looking for early signs of imbalance, postural changes, arthritis etc,. This is a great way to take preventative measures to sustain your care. Another option is, if you are anything like me, getting more fit is always at the top of my new year's resolutions list but I don't want to be in the gym when it is the most packed at the start of the year. Utilizing my extra FSA funds is a great way for me to kick start my fitness goals early, to balance out adding potencial holiday pounds. I work directly with my therapist (Dr. Gil Halfon) on a routine that is safe, practical and custom to my goals all while having the best, soothing, hands on manual (PT massages) this side of Brooklyn after my training sessions.
How to get started ?
We’re ready to help you move healthier, happier and pain free in 2022!
Call us today to schedule your appointment 1-718-258-3300 or find us online by clicking here or schedule via ZocDoc.com
About EvolveNY-
Brooklyn's Premier Holistic Physical Therapy Clinics- There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better! First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
https://EvolveNY.com
Physical Therapy for Neck Pain and Neck Injuries
Neck Physical Therapy: IS NECK PAIN INTERFERING WITH YOUR QUALITY OF LIFE? Whether it’s a new pain you are experiencing or an ongoing problem, discomfort in this area can be a literal pain in the neck. Hours sitting at your desk working each day, that fender bender you had last week, years of looking down while working on items with your hands can all lead to acute and chronic neck pain and stiffness and an amalgam of symptoms from headaches to arm weakness. While sometimes it may seem like these symptoms will never go away, physical therapy is an effective option to help reduce these symptoms that will also empower you to implement strategies to prevent them from recurring. This article will help you to understand the causes, symptoms and possible interventions that you can expect during a physical therapy treatment.
Neck Physical Therapy
IS NECK PAIN INTERFERING WITH YOUR QUALITY OF LIFE?
Whether it’s a new pain you are experiencing or an ongoing problem, discomfort in this area can be a literal pain in the neck. Hours sitting at your desk working each day, that fender bender you had last week, years of looking down while working on items with your hands can all lead to acute and chronic neck pain and stiffness and an amalgam of symptoms from headaches to arm weakness. While sometimes it may seem like these symptoms will never go away, physical therapy is an effective option to help reduce these symptoms that will also empower you to implement strategies to prevent them from recurring. This article will help you to understand the causes, symptoms and possible interventions that you can expect during a physical therapy treatment.
LET’S GET A BETTER UNDERSTANDING OF THE NECK AND HOW IT FUNCTIONS:
The neck, as we call it, is formally known as the cervical spine and is made up of 7 bony vertebrae that connect the bottom of the skull to the top of the upper back and ribcage. This area of the spine is made to be strong enough to support the weight of the skull and brain while still allowing for the many degrees of rotation, side bend, flexion and extension of the neck that we use daily. In between each vertebrae is an intervertebral disc which provides cushioning and shock absorption. Traveling through the bony spinal canal created by the vertebrae is the spinal cord which carries motor and sensory information to and from the brain to the rest of the body through nerves that exit the small canals created by the vertebrae on the left and right side.
There are many muscles that attach to the skull and neck bones and connect to lower vertebrae, the shoulder blades, the clavicle, and the upper ribs. Some muscles are more superficial--closer to the skin--that act as movers of the neck and other bones while other muscles lie deeper and act to stabilize the neck and head.
It is important to understand that while in some cases a specific anatomical structure may be primarily to blame for your neck pain or discomfort, often times the underlying cause is due to faulty movement patterns or an imbalance in the length and strength of surrounding muscles and your physical therapist at Evolve will be evaluating how you move as much as he or she is examining the structures of the neck.
WHAT MIGHT BE THE CAUSE OF YOUR SYMPTOMS?
Dysfunction occurring in the cervical spine can present in many different ways. Some people may experience localized pain or stiffness in the muscles or joints of the neck itself, others may primarily experience headaches while in some cases people will complain of what we call radicular symptoms in their arms, meaning pain, weakness or sensory disturbances that originate from the nerves exiting the neck vertebrae that manifest in the arms and hands.
The good news is, your physical therapist is well-trained to spot all of the contributing factors to help create a comprehensive treatment plan. To help you to better understand some of the causes of neck pain and how your physical therapist will treat them, here are some examples:
Whiplash: Whiplash occurs when neck muscles are strained and tendons are stretched in response to a quick and uncontrolled forward and backwards movement of the neck beyond its normal range of motion. Whiplash can occur as the result of a hard tackle in football or from being hit from behind by another car while waiting at a stoplight. Pain and stiffness may not set in right away but take a day or two to manifest. In the first few days after injury your physical therapy treatment will focus on protecting the injured tissues which may include wearing a soft neck collar, using ice or electrical stimulation for pain and passive range of motion. As your healing progresses your physical therapist may implement hands-on techniques like soft tissue or joint mobilizations and you will begin to perform exercises to stretch and strengthen affected muscles to restore normal motion.
Intervertebral Disc Herniation: Between the bones of the spine lie the intervertebral discs which provide height and cushioning. A herniation of the jelly-like center (nucleus) of the disc through the outer, tougher layer (annulus) is called a disc herniation and it can occur from a sudden trauma or due to gradual age-related changes in the disc. It can sometimes place pressure on the nerves where they exit the spinal canal causing pain both locally and at times, into remote areas such as the arms and hands. If severe enough it can cause changes in the sensation of the skin and strength of muscles in the arms. During your treatment your PT will be prescribing you a series of movements and exercises to help relieve the pressure on the nerves and optimize your movement patterns to minimize future discomfort. They may also implement manual therapy, hands-on techniques such as joint and soft tissue mobilization.
Cervicogenic Headache: Originating from the joints of the upper cervical spine, this condition often causes chronic headaches that radiate from the lower skull upwards and are perceived in the head and/or regions of the face. Cervicogenic headaches are characterized by pain on one side of the head (sometimes both sides), diffuse pain in the shoulder or arm on the same side and stiffness or reduced range of motion of the neck. Cervicogenic headaches may develop after a recent trauma such as a concussion or may be aggravated by specific neck movements or sustained postures. Physical therapy to treat these headaches might include modalities such as heat or electrical stimulation to reduce pain, education on ergonomics and posture to limit aggravation of neck structure, exercises, breathing techniques and stretches to balance the strength and flexibility of the neck muscles, and mobilization or manipulation of the joints in the cervical spine.
While neck pain can be disruptive to your daily life, conservative treatments such as physical therapy are often highly effective. A physical therapist at Evolve can help you get on the road to healing your neck pain. Our therapists do not just treat symptoms, but we get to the root of the cause. We strive to enable our patients to live pain free, and prevent the recurrence of related issues.
Click here for more information about neck physical therapy in Brooklyn
About EvolveNY-
Brooklyn’s Premier Holistic Physical Therapy Clinics-
There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
https://EvolveNY.com
Is Your Back Killing You?
Is Your Back Bothering You? Physical Therapy for Back Pain and Injury- Upper and lower back pain and injuries can occur in any number of anatomical structures that make up your back. Muscles, bones, nerves, fascia, ligaments, intervertebral discs and tendons weave together to form the back. Pain or discomfort in this area can arise from an acute injury to muscle or bone, or can develop over time in response to repetitive or faulty movement patterns or to muscle length and strength asymmetries. This article will help you to understand the causes, symptoms and possible treatments that you can expect during a physical therapy treatment.
Physical Therapy for Back Pain and Injury
ARE YOU LIVING WITH NEW OR CHRONIC BACK PAIN?
Upper and lower back pain and injuries can occur in any number of anatomical structures that make up your back. Muscles, bones, nerves, fascia, ligaments, intervertebral discs and tendons weave together to form the back. Pain or discomfort in this area can arise from an acute injury to muscle or bone, or can develop over time in response to repetitive or faulty movement patterns or to muscle length and strength asymmetries. This article will help you to understand the causes, symptoms and possible treatments that you can expect during a physical therapy treatment.
LET’S GET A BETTER UNDERSTANDING OF THE SPINE AND HOW IT FUNCTIONS:
The spine, made up of 34 bones forms, well, the backbone of the body. It provides stiffness and structure to the torso while still allowing for the flexibility and movement needed to perform our daily tasks. The seven vertebrae that make up the neck, known as the cervical spine, the 12 vertebrae that make up the mid back, or thoracic spine, and the 5 vertebrae that make up the lower back, or lumbar spine, create a long canal that houses the spinal cord. The spinal cord is made up of a bundle of nerves that arise from the brainstem and leave through channels between the bones of the spine to innervate and carry movement and sensation information between the brain and the rest of the body. The broad and flat sacral bones sit beneath the last lumbar vertebrae and act as connectors between the pelvic bones and the spine. Beneath that, lives the coccyx or tailbone.
There are many muscles that compose the back. Some muscles are more superficial--closer to the skin--and often help in moving or positioning the arms. Intermediate layers of muscles act on the ribcage to help with respiratory function and finally there is the deep layer of muscles which lie close to and help move the spine. Any of these anatomical structures may be involved in back pain or injury and your physical therapist will perform a series of tests and measures to help them to localize the cause.
It is important to understand that while in some cases, a specific anatomical structure may be primarily to blame for your back pain or discomfort such as a herniation at an intervertebral disc or a strain of a specific muscle but often times the underlying cause is due to faulty movement patterns and your physical therapist at Evolve will be evaluating how you move as much as he or she is examining the structures of the back.
WHAT MIGHT BE THE CAUSE OF YOUR BACK PAIN?
Back pain is often multifactorial. Your back pain might be due to an injury or irritation to one of the structures we talked about above but could also be related to how strong your hips are, how flexible your shoulders are, how often you perform certain activities and how well you control the movement of your body during everyday tasks. The good news is, your physical therapist is well-trained to spot all of the contributing factors to help create a comprehensive treatment plan. To help you to better understand some of the causes of back pain, here are some examples:
Muscle Strain: A pulled or strained muscle can result from a trauma such as a fall, unexpected twist or pull. It can also result from repetitively overloading muscles through less than ideal biomechanics. These overloaded muscles may eventually be unable to compensate for weakened or fatigued primary muscles leading to a muscle strain. Symptoms of a muscle strain include pain, swelling, bruising, stiffness and limited range of motion. When you come to physical therapy your PT will not only address the symptoms of the muscle strain through modalities such as ice, ultrasound and electrical stimulation but will work to correct any underlying biomechanical inefficiencies and muscle imbalances to prevent future injuries.
Intervertebral Disc Herniation: Between the bones of the spine lie the intervertebral discs which provide height and cushioning. A herniation of the jelly-like center (nucleus) of the disc through the outer, tougher layer (annulus) is called a disc herniation and it can occur from a sudden trauma or due to gradual age-related changes in the disc. It can sometimes place pressure on the nerves where they exit the spinal canal causing pain both locally and at times, into remote areas such as the legs or feet. If severe enough it can cause changes in the sensation of the skin and strength of muscles in the legs and even affect bowel and bladder function. During your treatment your PT will be prescribing you a series of movements and exercises to help relieve the pressure on the nerves and optimize your movement patterns to minimize future discomfort. You can also expect your PT will be educating you on this condition and how you can modify your activity in the meantime.
Sciatica: Sciatica refers to pain, burning, tingling, cramping, numbness and sometimes weakness that often begins in the buttock and travels down the back of the leg. It is caused by compression or irritation of the sciatic nerve that arises in the low back and travels down the posterior leg. With severe or prolonged compression or irritation muscle weakness can also occur. Your physical therapist will be assessing for a number of causes including disc herniations, misalignment of the pelvis, tightness in the hip or buttock muscles, narrowing of the spine or biomechanical problems before they begin treating you. Treatment may include manual therapy techniques to help restore normal movement and soft tissue mobility, self-stretching to improve muscle length, strengthening to address weakness and education on improving movement patterns.
While upper and lower back pain can be disruptive to your daily life, conservative treatments such as physical therapy are often highly effective. Physical therapists can identify the myriad of factors contributing to your specific back pain and provide you with a rehabilitation program to improve your symptoms now and help prevent them in the future. A physical therapist at Evolve can help you get on the road to healing your back pain. Our therapists do not just treat symptoms, but we get to the root of the cause. We strive to enable our patients to live pain free, and prevent the recurrence of related issues.
Are you or someone you know experiencing upper back pain or lower back pain? Call Evolve Physical Therapy in Brooklyn today to make an appointment. Our physical therapists will work with you to reduce the risk of complications, and help you get back to living your life to the fullest. Call- 1-718-258-3300 or visit- https://evolveny.com/physical-therapy/back-physical-therapy-brooklyn
About EvolveNY-
Brooklyn's Premier Holistic Physical Therapy Clinics- There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Brooklyn Physical Therapy Clinic Locations!
https://EvolveNY.com
Is Your Ankle Bothering You?
Need Ankle Physical Therapy? Try Ankle Physical Therapy Services in Brooklyn with Evolve PT. Ankle injuries can keep you down and out for a long time if untreated or treated incorrectly. The ankle is a complex joint, like the wrist, it’s made up of dozens of joints and over a hundred muscles, tendons, and ligaments. The ankle is a magnificent system, the duality of its responsibility is unmatched when compared to other joints…
Need Ankle Physical Therapy? Try Ankle Physical Therapy Services in Brooklyn with Evolve PT!
Ankle injuries can keep you down and out for a long time if untreated or treated incorrectly. The ankle is a complex joint, like the wrist, it’s made up of dozens of joints and over a hundred muscles, tendons, and ligaments. The ankle is a magnificent system, the duality of its responsibility is unmatched when compared to other joints. It has a need to be conforming and supple enough to contour to any uneven surface, as well as being rigid enough to be a springboard for running and jumping. Safe to say, there’s a lot going on here. Most ankle injuries boil down to where the stress is going, and often a part foot is working too hard. This strain can be as benign as inflammation, to tendinitis, or at the extreme tearing of the ligaments and bones. Let’s go two of the most common ankle injuries, including the mechanism of injury and treatment.
Ankle sprain-
The most common type of sprain happens when your foot rolls over itself. This generally happens with sports stepping on someone’s foot for example, but also can be from stepping wrong on an uneven surface or off a curb. This is called an inversion ankle sprain, dubbed by the direction the foot is moving. Depending on how much the ankle rolls, and often how much weight is going through your ankle in that position, will determine how bad the sprain is. Initially immobilizing your foot is important, as you’re susceptible to spraining it more. Common treatment after includes working on the muscles involved in the injury, strength, and balance training to recalibrate your ankle in positions where the ligaments will be active.
Plantar Fasciitis-
The plantar fascia serves as a support structure for your foot, it helps form your arch. It fans out from your heel to your toes. The area on your heel where it attaches can become inflamed, often with excessive weight or overuse typical in flat feet. In mild cases, a change in footwear and stretching are often enough. If the inflammation is bad enough, immobilization and reduction of activity are required. This injury can be a nag, but with proper assessment of your gait, arches, and exercise form, it can be well managed.
If you’re unlucky enough to break your ankle, thankfully most of the time they heal and recover like it never even happened. The two bones from your calf, tibia and fibula, are typically the area a fracture occurs. Treatment for the fracture can vary anywhere from a cast with immobilization, to surgical fixation keeping the fracture in place using screws and plates. Recovery depends on where the fracture occurred, and the technique to keep it in place. Typically, is starts off with a period of immobilization and reduction in weightbearing to allow things to heal. Once you’re able to start moving again, Physical Therapy is your best bet to regaining the normal motion and function of the foot. The time in a cast or boot, albeit brief, will typically result in atrophy of the supporting structures of the ankle. Proper range of motion and strength exercises will be paramount to the eventual function of the foot.
Ankle injures can be complicated, and proper assessment and treatment is key. Thankfully at Evolve PT, we’ve got you covered. From the latest in soft tissue techniques, to expert gait and running analysis, there is no reason your ankle injury has to keep you from doing the things you love.
Click here for more information about ankle physical therapy in Brooklyn
About EvolveNY-
NYC's Premier Holistic Physical Therapy Clinics-
There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
https://EvolveNY.com
“GOT TAPED?"
Got Taped? Top 5 benefits of getting strapped up with RockTape. Check out Head Physical Therapist Dr. Nathan Kind’s Top 5 benefits of getting strapped up with RockTape.Written By: Dr. Nathan Kind, Clinical Director, RockSteady Program Director, DPT, PT.
Top 5 Benefits of Getting Strapped Up With RockTape
Check out Head Physical Therapist Dr. Nathan Kind’s Top 5 benefits of getting strapped up with RockTape.
By: Dr. Nathan Kind, Clinical Director, RockSteady Program Director, DPT, PT
Let's first talk about what is RockTape?
RockTape is a brand of Kinesiology Tape. Kinesiology Tape was first developed in the late 1970s by Dr. Kenzo Kase, a Japanese chiropractor who wanted a tape that provided support but didn’t limit movement the way traditional athletic tapes do. The tape is typically really stretchy, water resistant, Hypoallergenic, and most would say cool to wear. If you’ve ever watched a volleyball game or a competitive bicycle race, you’ve probably seen it: strips of colorful tape splayed in patterns across shoulders, knees, backs, and abs. Some of the evidence based research and study results show taping creates space in joints in areas such as the knees and shoulders which helps reduce the chance of joint irritation. Physical therapists like myself have taping changes the information your sensory nervous system is sending about pain and compression in your body. It seems taping can change signals on pain pathways which makes it a useful treatment tool for many patients.
Improves circulation of blood and fluids which mitigates pain and swelling by improving blood and lymphatic flow in the taped area.
Supports weak zones by providing reinforced support to fatigued joints and muscles without limiting movement. Taping provides a mechanical effect which improves the slides and glides between tissue layers.
Re-educating muscles taping helps retrain muscles that have lost function or that have gotten used to an unhealthy way of working. This can protect patients against injury by “waking up” the muscles and reminding it to keep working.
Scar Tissue Management: taping can be used to gently pull on scar tissue, providing a low intensity, long duration stretch to the tight collagen that makes up scar tissue. Taping can improve the long-term appearance of scars after surgery or injury.
Got Pain ? How about Swelling and Bruising ? Need functional support in movement ? Click here to find out more about Kinesiotaping
Check the link below or call 1-718-258-3300 to learn more.
About EvolveNY-
Brooklyn's Premier Holistic Physical Therapy Clinics-
There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
WORKING FROM HOME CAUSING YOU BACK PAIN?
WORKING FROM HOME CAUSING YOU BACK PAIN? GET BACK ON TRACK! Reduce Back Pain while working from home. 4 Tips to Reduce Back Pain-If you’ve been working from home for a while and are noticing lower back pain that lingers, it could be caused by your home office set-up. Working longer hours, not having a supportive chair and poor posture can all lead to back pain. “The urgency in which people were sent home to work during the peak of the pandemic, left little to no time to set up a proper office space,” explains Dr. Nathan Kind, physical therapist at Evolve Sport Rehabilitation - Brooklyn. “Also, without the usual distractions of work, people find themselves sitting for 3-4 hours or more without getting up to run to various meeting room shared office spaces.
GET BACK ON TRACK! Reduce Back Pain While Working from Home.
4 Tips to Reduce Back Pain
If you’ve been working from home for a while and are noticing lower back pain that lingers, it could be caused by your home office set-up. Working longer hours, not having a supportive chair and poor posture can all lead to back pain. “The urgency in which people were sent home to work during the peak of the pandemic, left little to no time to set up a proper office space,” explains Dr. Nathan Kind, physical therapist at Evolve Sport Rehabilitation - Brooklyn. “Also, without the usual distractions of work, people find themselves sitting for 3-4 hours or more without getting up to run to various meeting room shared office spaces.
Extended sitting leads to poor posture, which can ultimately lead to pain. Nathan further explains that “The stress from juggling life at home can also increase pain from ramped up cortisol, tightness in muscles, shallow breathing and decreased circulation throughout the body,” Dr. Kind explains. “It’s been a perfect recipe of factors that contribute to back and neck pain.” Dr. Kind shares advice on how to get “back on track” reduce back pain while working from home.
Tips on How To Reduce Back Pain And Sciatica While Working From Home-
START YOUR DAY WITH A STRETCH!
Whether you’re suffering from pain in the lower back, mid-back, or upper back and shoulders, here are two stretches that are easy to try:
Knee to chest: Don’t be fooled by this stretch’s simplicity. This is a really effective way to stretch the hamstrings and lower back. Lie on your back with your legs flat on the floor. Gently bend one leg up, placing your hands over your knee to hold it in place. Hold this for 30 seconds on each leg.
Side bends: While standing, slowly slide your right hand down the side of your right leg, going as far as you can until you feel any stretch or discomfort. Hold for 10 seconds and ease yourself back to standing. Repeat on the left side.
VIEW YOUR COMPUTER SCREEN WITH A STRAIGHT NECK!
Put your screen in front of you at a comfortable viewing height. Don’t look down at your screen, like to a laptop on a table or to your phone. And don’t angle your screen so you must twist your neck–some people like to put their keyboard and mouse in front of them with their screen off to the side, but then they end up dealing with neck pain from the swiveling. If you have a separate screen or if you are using a laptop, you might have to put it on a pile of books or on a cardboard box to raise it to a comfortable viewing position straight in front of you.
STAY HYDRATED!
Simple, yet often forgotten when we get busy, remember to keep up your water intake. Drinking plenty of water helps keep your muscles and skin well hydrated. It ensures the body has plenty of opportunities to take away waste products from the muscles that are working hard keeping you in your forced typing/desk position. There are also secondary benefits too. You have to get up out of your seat to get a refill, giving you a natural break and, most likely, you will be going to the loo more often!
SCHEDULE TIME FOR YOUR BODY TO MOVE!
When we asked Dr. Kind, what’s the most important advice you can give someone working from home ? He replied “ Take a shake break, take a break simply just to move and schedule time to take care of your body”.
The Key is not to stay in any one position for longer than about 45 minutes. Get up and move around be intentional about your movement. If you have a smartwatch or Fitbit wear it and follow the prompts to stretch.
If you need help with getting back on track schedule Physical Therapy as part of your weekly fitness/wellness routine. There are a lot of simple exercises we can teach you to do at home or at work to strengthen your core and support your lower back and spine.
Got Sciatica? Do you have an excruciating pain or electrical shock feeling running down your back and legs that just won't quit? Check Out Some of Evolve Physical Therapy’s Lower Back Stretches and Sciatica Specific Stretches…
Got Pain? Schedule a Consultation Today! Walk Ins Welcome.
Got lower back pain and/or Sciatica? Call us today to schedule an appointment! Call- 1-718-258-3300
About Evolve Physical Therapy in Brooklyn-
There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of bio-mechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
What is Instrument Assisted Soft Tissue Mobilization
Instrument Assisted Soft Tissue Mobilization-Instrument Assisted Soft Tissue Mobilization, or IASTM, is a tool that therapists may use to treat soft tissue dysfunction. This approach to soft tissue work is utilized to identify and treat restrictions in the fascia. IASTM tools are designed to find tissue abnormalities such as scars, restrictions and adhesions. The tools are made to allow the therapist to concentrate their force into a smaller surface area, resulting in a more efficient treatment. The goal of using these tools is to trigger an inflammatory healing response in order to stimulate the production of new collagen and encourage pain free healing.
Instrument Assisted Soft Tissue Mobilization
Instrument Assisted Soft Tissue Mobilization, or IASTM, is a tool that therapists may use to treat soft tissue dysfunction. This approach to soft tissue work is utilized to identify and treat restrictions in the fascia. IASTM tools are designed to find tissue abnormalities such as scars, restrictions and adhesions. The tools are made to allow the therapist to concentrate their force into a smaller surface area, resulting in a more efficient treatment. The goal of using these tools is to trigger an inflammatory healing response in order to stimulate the production of new collagen and encourage pain free healing.
Some issues that it may be used for are:
Chronic Inflammation
Cervical or lumbar sprains
Plantar Fasciitis
Scar Tissue
Trigger Finger
Patellofemoral disorders
Myofascial pain and restrictions
IT Band Syndrome
Although controversial, there have been multiple studies addressing the benefits of IASTM on a cellular level. Some of these include reduction in scar tissue, an increase in circulation, and remodeling of collagen fibers to promote healing and restore function. When IASTM is incorporated into a therapeutic exercise program, the soft tissue is encouraged to lay itself down in an appropriate arrangement.
What Should I Expect From an IASTM treatment?
Your therapist will use their instrument to glide over your skin. When the tool picks up on scar tissue or an adhesion, you will feel a “catch”. Your therapist will then spend about 30-90 seconds treating this area. IASTM should not be painful but it may be uncomfortable at times. After your trouble area is treated, your therapist will guide you through a stretching or strengthening program, depending on your needs.
The potential outcomes from this type of treatment include increased range of motion, blood flow, and decreased pain. Mild soreness following a treatment is not uncommon and is not dangerous. When paired with active exercises, IASTM is an effective tool that your physical therapist may utilize to help you gain the maximum benefits from your treatment sessions. Give us a call to schedule an appointment- 1-718-258-3300 or click here to find out more about IASTM physical therapy services.
About Evolve Physical Therapy-
There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
What is Complex Regional Pain Syndrome?
What is Complex Regional Pain Syndrome? Complex Regional Pain Syndrome is a disproportionate response of the sympathetic nervous system (think fight or flight) following an injury. This abnormal feedback to the brain has been associated with injuries to bone, nerve, soft tissue, and blood vessels. It is most commonly seen in the hand and foot after immobilizing a painful injury in that region or after a stroke or heart attack.
What is Complex Regional Pain Syndrome?
Complex Regional Pain Syndrome is a disproportionate response of the sympathetic nervous system (think fight or flight) following an injury. This abnormal feedback to the brain has been associated with injuries to bone, nerve, soft tissue, and blood vessels. It is most commonly seen in the hand and foot after immobilizing a painful injury in that region or after a stroke or heart attack.
Someone who has Complex Regional Pain Syndrome (CRPS) will complain of a continuous throbbing or burning pain in their arm, hand, leg, or foot. They may have increased sensitivity to touch, cold, and have changes to their skin color. These skin changes can range from blue, to red, to white blotches. The joints affected may be stiff and swollen as well. People with this syndrome may experience muscle spasms, tremors, and weakness.
There are two types of CRPS that one can develop:
Type 1: This type is found in the vast majority of CRPS patients, about 90%. It occurs after an injury that did not directly damage any nerves in the affected region.
Type 2: This less common form occurs after a direct injury to a nerve in the affected limb.
There is no general timeline for symptoms of this condition as it can last anywhere from a few months to a year. CRPS can lead to ongoing chronic pain which is a potential risk factor for developing clinical psychological depression.
Early management is crucial in order to support a good prognosis. There are some disabling complications that can develop if this issue is not taken care of early enough. The most common ones include muscle wasting and muscle contractures. When you visit your doctor, they will direct your treatment toward disrupting the increased sympathetic response and a nerve block medication will likely be administered. While medication will help ease the pain, it does not provide long term relief.
While medicated, it is important to see a physical therapist who will help you exercise through pain free ranges of motion. A physical therapist will help you loosen up joints that are stiff in order to prevent muscle and joint deterioration. They will also work with you to reduce the risk of contractures, which is caused by the tightening of muscles. In addition, various therapeutic techniques may be utilized to reduce swelling and reduce pain.
Medication alone will not help someone with CRPS get better for the long run. However, it significantly improves a patient’s ability to cooperate and perform better in a physical therapy session.
Are you or someone you know experiencing CRPS? Call us today to make an appointment. Our therapists will work with you to reduce the risk of complications, and help you get back to living your life to the fullest. Call to schedule an appointment! 1-718-258-3300
About Evolve Physical Therapy in Brooklyn-
Brooklyn's Premier Holistic Physical Therapy Clinics:
There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!
Upper Back Strain?
Upper Back Strains- If you are experiencing pain on your upper back, specifically between your shoulder blades, you may have a rhomboid strain or spasm. The rhomboids are muscles that pull your shoulders back and rotate your scapulae down. They also act as a stabilizer, positioning the scapulae onto the thoracic wall. Activation of these muscles help to maintain proper posture while standing, sitting, and walking. When not activated, the shoulders can protrude forward, leading to poor posture and upper back pain.
Upper Back Strains
If you are experiencing pain on your upper back, specifically between your shoulder blades, you may have a rhomboid strain or spasm. The rhomboids are muscles that pull your shoulders back and rotate your scapulae down. They also act as a stabilizer, positioning the scapulae onto the thoracic wall. Activation of these muscles help to maintain proper posture while standing, sitting, and walking. When not activated, the shoulders can protrude forward, leading to poor posture and upper back pain.
A rhomboid strain or spasm is usually caused from repetitive motions or other overuse of the shoulder. Some of these include overhead activities such as pitching, serving a tennis ball, rowing, carrying a heavy load such as a backpack, and sustained poor posture for long periods of time. A strain may cause pain in between your shoulder blades and can be assessed by your physical therapist.
Your physical therapist will help you strengthen and stretch the muscles in your upper back and shoulders in order to correct any existing muscle imbalances and to improve your posture. They also may incorporate some modalities into your treatment such as ice, ultrasound, and soft tissue work. All of these approaches will work off of one another to manage pain and inflammation. In order to facilitate the healing process, you will need to modify your activities in order to avoid anything that aggravates your upper back pain. Your PT will most likely prescribe a home exercise program to complete between visits. You and your physical therapist will become partners in your healing; they will give you the tools you need to get yourself better in a timely manner. Following this plan is important to speed up recovery. A mild strain should heal within 4-6 weeks while more severe strains may take longer.
There are a few actions you can take to prevent rhomboid muscle strains or spasms:
Be sure to warm up and cool down before and after your workouts
Perform dynamic stretches before activity and static stretches after activity
If you have a desk job, set an alarm on your device to remind you to take breaks and move around every 45 minutes
Practice proper technique while playing sports
If you wear a backpack, make sure to carry it on both shoulders
Here are some exercises that can help with upper back pain due to rhomboid sprains and spasms:
Shoulder Retractions: Sit or stand with your arms at your sides. Draw your shoulder blades together while bringing them down and back. Hold this position for 5 seconds and repeat for 1 minute
Rhomboid Stretch: Extend your arms out in front of you, stacking your right hand over your left. Hold this position for 30 seconds and then switch sides. Repeat for a total of 3 times on each side.
Neck Rotations: Sit upright at the edge of a chair. Inhale while turning your head to the right and hold at the end of your range for 30 seconds while taking deep breaths. Repeat on the left side. Do this for a total of 3 times on each side.
Got upper back pain? Call us today to make an appointment! Call- 1-718-258-3300
About Evolve Physical Therapy in Brooklyn-
Got Pain? Schedule a Consultation Today! Walk Ins Welcome.
There’s physical therapy, there’s training, and then there’s EVOLVE. We use the science of biomechanics merged with fitness to help our patients get better and stay better!
First we evaluate, then we heal, then we strengthen our clients so they can reach their goals, feel better, and live happier lives. We do so by utilizing a range of core techniques and specialized treatments to reduce pain, improve mobility, enhance physical strength and deal with the underlying issues, not just the pain itself.
Multiple Locations!